What Is a DNR?
Nurses need to know what is a DNR, how it is created, who can sign it, and what their responsibility is regarding a DNR order.
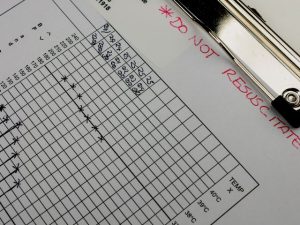
Ideally it is a legal document and found in the patient’s medical chart. Unfortunately, many times a written and signed order is hard to locate and without it, the medical team is legally and medically responsible to provide life saving measures when a patient’s heart stops.
Some facilities have a policy that a nurse who is caring for the client cannot be one of the witnesses, but that varies among facilities.
Every time a person is admitted to a hospital, including an ER visit, nurses should ask if the person has a living will, or advance directives.
Advance directives is an umbrella term for legal forms that direct the medical staff in advance of a client’s inability to voice a preference for end-of-life procedures due to an injury or serious illness.
Three forms are included under advance directives and include the DNR form, the living will, and durable power of attorney. The DNR form states the person’s desire for or against cardiopulmonary resuscitation. The living will is a general term voicing the person’s preferences.
An example of a common statement found in a living will is: “If I suffer an incurable, irreversible illness, disease, or condition and my attending physician determines that my condition is terminal, I direct that life-sustaining measures that would serve only to prolong my dying be withheld or discontinued.” The durable power of attorney for medical decisions names someone to make decisions for them if the person is unable to do so.