Diagnostic Process for Myocardial Infarction
Causes of Myocardial Infarction
Myocardial infarctions can occur due to various reasons; however, the most common cause is coronary thrombosis of a coronary artery narrowed with plaque.
Other causes include the following:
- Spasms of the coronary arteries
- Blockage of the coronary arteries by embolism or thrombi
- Fatty plaques
- Air
- Calcium deposits
- The disparity between myocardial oxygen demand and coronary arterial supply
Risk Factors for Myocardial Infarction
The unmodifiable risk factors for coronary artery disease and myocardial infarction include:
The modifiable risk factors include:
- Cigarette smoking, which causes arterial vasoconstriction and increased plaque formation.
- A diet high in saturated fats, cholesterol, sugar, salt, and total calories can increase the risk of a myocardial infarction.
- Elevated serum cholesterol and low-density lipoprotein levels can increase the risk of atherosclerosis.
- Obesity and hypertension can increase the workload of the heart.
- Diabetes mellitus can decrease blood circulation to the heart muscle.
- Mental and emotional stress can activate the sympathetic nervous system and increase the risk of heart disease.
- A sedentary lifestyle can decrease the blood circulation and strength of the cardiac muscle.
- Medications can also increase the risk of heart disease, such as oral contraceptives may enhance thrombus formation, cocaine use can cause coronary artery spasms, and anabolic steroid use can accelerate atherosclerosis.
Nursing Assessment
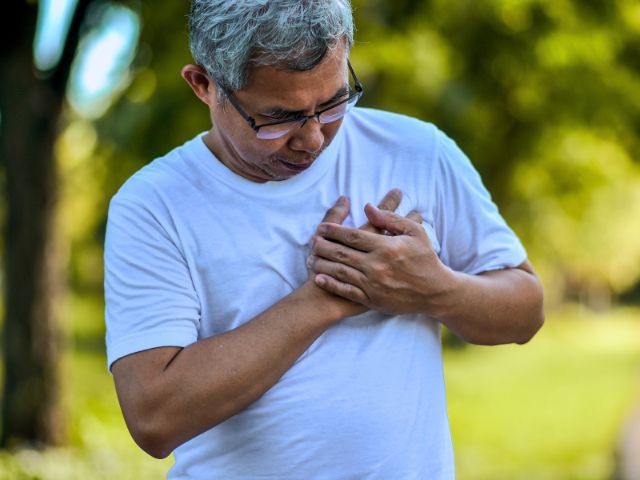
To finalize the diagnosis of myocardial infarction, you need to keep a close watch on the symptoms. If you suspect the patient has myocardial infarction, ask the following questions regarding pain:
- Chest pain
- Jaw pain
- Arm pain
- Epigastric pain
It is important to remember that some patients have no pain at all. In these instances, evaluate the entire clinical picture and ask the patient about other clinical symptoms such as shortness of breath, racing heart rate, diaphoresis, clammy skin, dizziness, nausea, and vomiting. It is imperative to be aware that sudden death and full cardiac arrest may be the first indication of myocardial infarction.
Elicit a thorough description of the symptoms using the P, Q, R, S, T approach where the letters indicate the following:
- P stands for palliative or precipitating measures. Ask the patient what was occurring and what made the symptoms worse. Did anything help in getting the symptoms better?
- Q stands for the quality of discomfort. Ask the patient if the pain was sharp, stabbing, or feeling like pressure.
- R indicates radiating. Ask the patient if the pain was radiating somewhere to another organ.
- S represents the severity of the pain, ranging on a scale of 1 to 10.
- T stands for time, from when the pain, symptoms, and discomfort began. Time management is a crucial step in treating a patient with myocardial infarction because the delay in giving medical care means more muscle damage occurs. The timing of asking these questions is also important; however, if the patient is in acute distress, ask only necessary questions. In this way, you can treat the patient effectively and ask additional questions later.
Physical Examination
The patient with myocardial infarction may have the following signs and symptoms:
- Chest discomfort
- Diaphoresis
- Clammy skin
- Nausea and vomiting
- Shortness of breath
- Epigastric discomfort
The pain is often intense and continuous for 30 to 60 minutes and may radiate up the neck and into the shoulder and jaw area. It may also vary in intensity. Some patients describe the pain as aching, burning, stabbing, or squeezing; however, some patients only have mild discomfort.
Observe the patient’s respiratory status, including depth, rate, rhythm, and effort. Also, observe their skin for color and diaphoresis and their mental status for confusion, dizziness, and anxiety. When you auscultate the patient’s heart, you may hear irregular sounds, especially if dysrhythmia is present.
Diagnostic Highlights
To diagnose a patient with myocardial infarction, the following diagnostic tests can be helpful:
Creatine kinase isoenzyme (MB-CK)
The normal reading is 0% – 6% of the total CK. In abnormal conditions, the levels are raised, which indicates tissue damage.
Cardiac troponin I (cTnI) and cardiac troponin T (cTnT)
- Normal results range between 3.1 g/L and 0.2 g/L, respectively. When the results are abnormal, it is elevated.
- Cardiac troponin levels have the highest specificity and sensitivity compared to CK-MB levels for detecting a myocardial infarction. It is also used to differentiate between angina and myocardial infarction.
- The earliest increase in the level occurs from the onset of chest pain in 3 to 6 hours. Peak increase occurs in 10 to 48 hours. Serum levels return to baseline at 5 to 14 days.
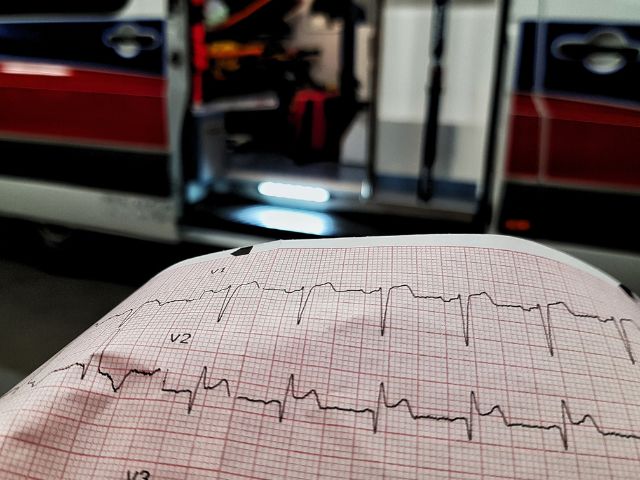
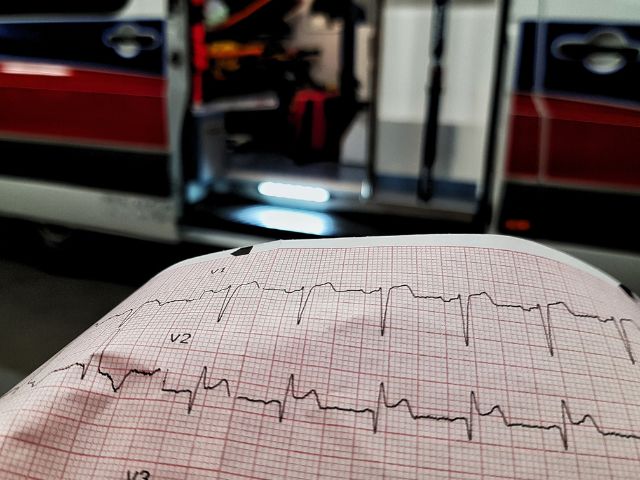
Electrocardiogram
- Under normal conditions, an electrocardiogram (ECG) shows a normal PQRST pattern; however, when there is an abnormality, it shows an ST-segment elevation, T wave inversion, and an abnormal Q wave (wider than 0.04 seconds or more than 1/3 height of the QRS complex) or STEMI (where ST elevation indicates myocardial infarction).
- ECG remains an effective tool in the diagnosis of myocardial infarction because the electrical conduction system is negatively affected due to myocardial ischemia and necrosis. A Q wave occurs because necrotic cells do not conduct electrical stimuli.
Other important tests that may need to be completed for a patient with myocardial infarction are as follows:
- Cholesterol (total, low-density lipoprotein, high-density lipoprotein) and serum triglycerides
- Lactate dehydrogenase
- C-reactive protein
- Complete blood count
- Serum myoglobin
- Cardiac catheterization
- Thallium scan
- Radionuclide ventriculography
- Two-dimensional echocardiography
Psychosocial
Ask the patient about any stressors in their life and the coping mechanisms used for these stressors. A diagnosis of a myocardial infarction can be overwhelming and life-changing for the patient; therefore, counsel and guide the patient with lifestyle changes they can successfully make.
Planning and Implementation
- The primary treatment goals for the patient with myocardial infarction are to restore the balance of oxygen supply and demand, relieve the pain associated with it, and prevent its complications.
- In route to the hospital, administer IV aspirin to the patient due to its antiplatelet effects. For active chest pain, you can give nitroglycerin once ordered by the physician. The physician usually prescribes oxygen therapy, often at 2 to 4 L/min to provide increased oxygen to the myocardial tissue.
- If it has been less than 4 to 6 hours since the pain began and you suspect MI, thrombolytics can be useful. Second-generation fibrinolytic drugs such as tenecteplase have clot selectivity and are often used to treat patients with myocardial infarction.
- When the patient is stabilized, cardiac catheterization can then be conducted. Keep a keen eye on the patient’s health and notify the physician for significant signs of decreased cardiac output such as hypotension, diminished urine output, crackles in the lungs, cool and clammy skin, and fatigue.
- The surgical option for plaque removal in the coronary artery is coronary artery bypass grafting (CABG). With treatment, diet restriction should be started at the hospital and followed at home as well. The patient, along with the dietician, physician, and nurse, plans for a diet low in cholesterol, fat, sodium, calories, and triglycerides.
- After giving immediate treatment, the focus is to manage chest pain and other symptoms associated with myocardial infarction.
- During the recovery phase, reduce the oxygen demand of the myocardial tissue and teach the patient and family about recovery.
- Remember that chest pain may indicate continued tissue damage; therefore, manage chest pain immediately.
- With pharmacological treatment, other measures can also be taken to reduce the preload of the heart and lower chest pain. Encourage the patient to have bed rest for at least the first 24 hours post angina or myocardial infarction.
- Create a peaceful and soothing environment for the patient to rest and encourage the family to take care of the patient while they rest. Ask the patient to not exert or perform straining activities such as Valsalva’s maneuver.
- After a myocardial infarction, anxiety, and panic levels are quite high among the patient and family members. Encourage them to discuss their concerns with you. Explain everything to them in a calm and reassuring voice. If possible, stay with the patient during periods of high anxiety.
- Discuss with the patient and family the diagnosis, activity, diet restrictions, and medical treatment. The patient may need numerous lifestyle changes. A cardiac rehabilitation program can be helpful for the patient in giving them emotional and social support, encouragement, and guidance.
- The cardiac rehabilitation program aims to reduce the recurrence of another attack and to improve the quality of life of the patient, done through reeducation and implementation of a secondary prevention program. The program provides the patient with the appropriate education, guidance, psychosocial support, and monitored exercise. To determine the exercise, the patient has to undergo an exercise stress test. It is completed to understand the patient’s response to physical activity. Usually, there are three phases to cardiac rehabilitation: in-hospital, outpatient, and follow-up.