Course
Wisconsin APRN Bundle
Course Highlights
- In this Wisconsin APRN Renewal Bundle course, we will learn about factors when prescribing opioids, indications, and effects.
- You’ll also learn the action of non-insulin injectable diabetes medication semaglutide.
- You’ll leave this course with a broader understanding of common side effects, including severe possible side effects, of medications used to manage asthma.
About
Pharmacology Contact Hours Awarded: 16
Course By:
Various Authors
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Controlled Substances
Introduction
Pain is complex and subjective. The experience of pain can significantly impact an individual’s quality of life. According to the National Institute of Health (NIH) (40), pain is the most common complaint in a primary care office, with 20% of all patients reporting pain. Chronic pain is the leading cause of disability, and effective pain management is crucial to health and well-being, particularly when it improves functional ability. Effective pain treatment starts with a comprehensive, empathic assessment and a desire to listen and understand. Nurse Practitioners are well-positioned to fill a vital role in providing comprehensive and empathic patient care, including pain management (23).
While the incidence of chronic pain has remained a significant problem, how clinicians manage pain has significantly changed in the last decade, primarily due to the opioid epidemic. This education aims to discuss pain and the assessment of pain, federal guidelines for prescribing, the opioid epidemic, addiction and diversion, and recommendations for managing pain.
Definition of Pain
Understanding the definition of pain, differentiating between various types of pain, and recognizing the descriptors patients use to communicate their pain experiences are essential for Nurse practitioners involved in pain management. By understanding the medical definition of pain and how individuals may communicate it, nurse practitioners can differentiate varying types of pain to target assessment.
According to the International Association for the Study of Pain (27), pain is “an unpleasant sensory and emotional experience associated with actual or potential tissue damage or terms of described such in damage.” The IASP, in July 2020, expanded its definition of pain to include context further.
Their expansion is summarized below:
- Pain is a personal experience influenced by biological, psychological, and social factors.
- Pain cannot be inferred solely from activity in sensory neurons.
- Individuals learn the concept of pain through their life experiences.
- A person’s report of an experience in pain should be respected.
- Pain usually serves an adaptive role but may adversely affect function and social and psychological well-being.
- The inability to communicate does not negate the possibility of the experience of pain.


Self Quiz
Ask yourself...
- Analyze how changes to the definition of pain may affect your practice.
- Discuss how you manage appointment times, knowing that 20% of your scheduled patients may seek pain treatment.
- How does the approach to pain management change in the presence of a person with a disability?
Types of Pain
Pain originates from different mechanisms, causes, and areas of the body. As a nurse practitioner, understanding the type of pain a patient is experiencing is essential for several reasons (23).
- Determining an accurate diagnosis. This kind of pain can provide valuable clues to the underlying cause or condition.
- Creating a treatment plan. Different types of pain respond better to specific treatments or interventions.
- Developing patient education. A nurse practitioner can provide targeted education to patients about their condition, why they may experience the pain as they do, its causes, and treatment options. Improving the patient's knowledge and control over their condition improves outcomes.
Acute Pain
Acute pain is typically short-lived and is a protective response to an injury or illness. Patients are usually able to identify the cause. This type of pain resolves as the underlying condition improves or heals (12).
Chronic Pain
Chronic pain is diagnosed when it continues beyond the expected healing time. Pain is defined as chronic when it persists for longer than three months. It may result from an underlying disease or injury or develop without a clear cause. Chronic pain often significantly impacts a person's physical and emotional well-being, requiring long-term management strategies. The prolonged experience of chronic pain usually indicates a central nervous system component of pain that may require additional treatment. Patients with centralized pain often experience allodynia or hyperalgesia (12).
Allodynia is pain evoked by a stimulus that usually does not cause pain, such as a light touch. Hyperalgesia is the effect of a heightened pain response to a stimulus that usually evokes pain (12).
Nociceptive Pain
Nociceptive pain arises from activating peripheral nociceptors, specialized nerve endings that respond to noxious stimuli. This type of pain is typically associated with tissue damage or inflammation and is further classified into somatic and visceral pain subtypes.
Somatic pain is most common and occurs in muscles, skin, or bones; patients may describe it as sharp, aching, stiffness, or throbbing.
Visceral pain occurs in the internal organs, such as indigestion or bowel spasms. It is more vague than somatic pain; patients may describe it as deep, gnawing, twisting, or dull (12).
Neuropathic pain
Neuropathic pain is a lesion or disease of the somatosensory nervous system. Examples include trigeminal neuralgia, painful polyneuropathy, postherpetic neuralgia, and central poststroke pain (10).
Neuropathic pain may be ongoing, intermittent, or spontaneous pain. Patients often describe neuropathic pain as burning, prickling, or squeezing quality. Neuropathic pain is a common chronic pain. Patients commonly describe allodynia and hyperalgesia as part of their chronic pain experience (10).
Affective pain
Affective descriptors reflect the emotional aspects of pain and include terms like distressing, unbearable, depressing, or frightening. These descriptors provide insights into the emotional impact of pain on an individual's well-being (12).

Self Quiz
Ask yourself...
- How can nurse practitioners effectively elicit patient descriptors to accurately assess the type of pain the patient is experiencing?
- Expand on how pain descriptors can guide interventions even if the cause is not yet determined.
- What strategies ensure patients feel comfortable describing their pain, particularly regarding subjective elements such as quality and location?
Case Study
Mary Adams is a licensed practical nurse who has just relocated to town. Mary will be the utilization review nurse at a local long-term care facility. Mary was diagnosed with Postherpetic Neuralgia last year, and she is happy that her new job will have her mostly doing desk work and not providing direct patient care as she had been before the relocation. Mary was having difficulty at work at her previous employer due to pain. She called into work several times, and before leaving, Mary's supervisor had counseled her because of her absences.
Mary wants to establish primary care immediately because she needs ongoing pain treatment. She is hopeful that, with her new job and pain under control, she will be able to continue a successful career in nursing. When Mary called the primary care office, she specifically requested a nurse practitioner as her primary care provider because she believes that nurse practitioners tend to spend more time with their patients.
Assessment
The assessment effectively determines the type of treatment needed, the options for treatment, and whether the patient may be at risk for opioid dependence. Since we know that chronic pain can lead to disability and pain has a high potential to negatively affect the patient's ability to work or otherwise, be productive, perform self-care, and potentially impact family or caregivers, it is imperative to approach the assessment with curiosity and empathy. This approach will ensure a thorough review of pain and research on pain management options. Compassion and support alone can improve patient outcomes related to pain management (23).
Record Review
Regardless of familiarity with the patient, reviewing the patient's treatment records is essential, as the ability to recall details is unreliable. Reviewing the records can help identify subtle changes in pain description and site, the patient's story around pain, failed modalities, side effects, and the need for education, all impacting further treatment (23).
Research beforehand the patient's current prescription and whether or not the patient has achieved the maximum dosage of the medication. Analysis of the patient's past prescription could reveal a documented failed therapy even though the patient did not receive the maximum dose (23).
A review of documented allergens may indicate an allergy to pain medication. Discuss with the patient the specific response to the drug to determine if it is a true allergy, such as hives or anaphylaxis, or if the response may have been a side effect, such as nausea and vomiting.
Research whether the patient tried any non-medication modalities for pain, such as physical therapy (PT), occupational therapy (OT), or Cognitive Behavioral Therapy (CBT). Note any non-medication modalities documented as failed therapies. The presence of any failed therapies should prompt further discussion with the patient, family, or caregiver about the experience. The incompletion of therapy should not be considered failed therapy. Explore further if the patient abandoned appointments.
Case Study
You review the schedule for the week, and there are three new patient appointments. One is Mary Adams. The interdisciplinary team requested and received Mary's treatment records from her previous primary care provider. You make 15 minutes available to review Mary's records and the questionnaire Mary filled out for her upcoming appointment. You see that Mary has been diagnosed with Postherpetic Neuralgia and note her current treatment regimen, which she stated was ineffective. You write down questions you will want to ask Mary. You do not see evidence of non-medication modalities or allergies to pain medication.

Self Quiz
Ask yourself...
- What potential risks or complications can arise from neglecting to conduct a thorough chart review before initiating a pain management assessment?
- In your experience, what evidence supports reviewing known patient records?
- What is an alternative to reviewing past treatment if records are not available?
Pain Assessment
To physically assess pain, several acronyms help explore all the aspects of the patient's experience. Acronyms commonly used to assess pain are SOCRATES, OLDCARTS, and COLDERAS. These pain assessment acronyms are also helpful in determining treatment since they include a character and duration of pain assessment (23).
| O-Onset | S-Site | C-Character |
| L-Location | O-Onset | O-Onset |
| D-Duration | C-Character | L-Location |
| C-Character | R-Radiate | D-Duration |
| A-Alleviating | A-Associated symptoms | E-Exacerbating symptoms |
| R-Radiating, relieving | T-Time/Duration | R-Relieving, radiating |
| T-Temporal patterns (frequency) | E-Exacerbating | A-Associated symptoms |
| S-Symptoms | S-Severity | S-Severity of illness |
Inquire where the patient is feeling pain. The patient may have multiple areas and types of pain. Each type and location must be explored and assessed. Unless the pain is from a localized injury, a body diagram map, as seen below, is helpful to document, inform, and communicate locations and types of pain. In cases of Fibromyalgia, rheumatoid arthritis, or other centralized or widespread pain, it is vital to inquire about radiating pain. The patient with chronic pain could be experiencing acute pain or a new pain site, such as osteoarthritis, that may need further evaluation and treatment (23).
Inquire with the patient how long their pain has been present and any associated or known causative factors. Pain experienced longer than three months defines chronic versus acute pain. Chronic pain means that the pain is centralized or a function of the Central Nervous system, which should guide treatment decisions.
To help guide treatment, ask the patient to describe their pain. The description helps identify what type of pain the patient is experiencing: Allodynia and hyperalgesia indicate centralized pain; sharp, shooting pain could indicate neuropathic pain. Have the patient rate their pain. There are various tools, as shown below, for pain rating depending on the patient's ability to communicate. Not using the pain rating number alone is imperative. Ask the patient to compare the severity of pain to a previous experience. For example, a 1/10 may be experienced as a bumped knee or bruise, whereas a 10/10 is experienced on the level of a kidney stone or childbirth (23).
Besides the 0-10 rating scale and depending on the patient's needs, several pain rating scales are appropriate. They are listed below.
The 0-5 and Faces scales may be used for all adult patients and are especially effective for patients experiencing confusion.
The Defense and Veterans Pain Rating Scale (DVPRS) is a five-item tool that assesses the impact of pain on sleep, mood, stress, and activity levels (20).
For patients unable to self-report pain, such as those intubated in the ICU or late-stage neurological diseases, the FLACC scale is practical. The FLACC scale was initially created to assess pain in infants. Note: The patient need not cry to be rated 10/10.
| Behavior | 0 | 1 | 2 |
| Face | No particular expression or smile | Occasional grimace or frown, withdrawn, disinterested | Frequent or constant quivering chin, clenched jaw |
| Legs | Normal position or relaxed | Uneasy, restless, tense | Kicking or legs drawn |
| Activity | Lying quietly, in a normal position, or relaxed | Squirming, shifting back and forth, tense | Arched, rigid, or jerking |
| Cry | No cry wake or asleep | Moans or whimpers: occasional complaints | Crying steadily, screams, sobs, frequent complaints |
| Consolability | Content, relaxed | Distractable, reassured by touching, hugging, or being talked to | Difficult to console or comfort |
(21).
Assess contributors to pain such as insomnia, stress, exercise, diet, and any comorbid conditions. Limited access to care, socioeconomic status, and local culture also contribute to the patient's experience of pain (23). Most patients have limited opportunity to discuss these issues, and though challenging to bring up, it is compassionate and supportive care. A referral to social work or another agency may be helpful if you cannot explore it fully.
Assess for substance abuse disorders, especially among male, younger, less educated, or unemployed adults. Substance abuse disorders increase the likelihood of misuse disorder and include alcohol, tobacco, cannabis, cocaine, and heroin (29).
Inquire as to what changes in function the pain has caused. One question to ask is, "Were it not for pain, what would you be doing?" As seen below, a Pain, Enjoyment, and General Activity (PEG) three-question scale, which focuses on function and quality of life, may help determine the severity of pain and the effect of treatment over time.
| What number best describes your pain on average in the past week? 0-10 |
| What number best describes how, in the past week, pain has interfered with your enjoyment of life? 0-10 |
| What number determines how, in the past week, pain has interfered with your general activity? 0-10 |
(21).
Assess family history, mental health disorders, chronic pain, or substance abuse disorders. Each familial aspect puts patients at higher risk for developing chronic pain (23).
Evaluate for mental health disorders the patient may be experiencing, particularly anxiety and depression. The Patient Health Questionnaire (PHQ4) is a four-question tool for assessing depression and anxiety.
In some cases, functional MRI or imaging studies effectively determine the cause of pain and the treatment. If further assessment is needed to diagnose and treat pain, consult Neurology, Orthopedics, Palliative care, and pain specialists (23).
Case Study
You used OLDCARTS to evaluate Mary's pain and completed a body diagram. Mary is experiencing allodynia in her back and shoulders, described as burning and tingling. It is exacerbated when she lifts, such as moving patients at the long-term care facility and, more recently, boxes from her move to the new house. Mary has also been experiencing anxiety due to fear of losing her job, the move, and her new role. She has moved closer to her family to help care for her children since she often experiences fatigue. Mary has experienced a tumultuous divorce in the last five years and feels she is still undergoing some trauma.
You saw in the chart that Mary had tried Gabapentin 300 mg BID for her pain and inquired what happened. Mary explained that her pain improved from 8/10 to 7/10 and had no side effects. Her previous care provider discontinued the medication and documented it as a failed therapy. You reviewed the minimum and maximum dosages of Gabapentin and know Mary can take up to 1800mg/day.
During the assessment, Mary also described stiffness and aching in her left knee. She gets a sharp pain when she walks more than 500 steps, and her knee is throbbing by the end of the day. Mary rated the pain a 10/10, but when she compared 10/10 to childbirth, Mary said her pain was closer to 6/10. Her moderate knee pain has reduced Mary's ability to exercise. She used to like to take walks. Mary stated she has had knee pain for six months and has been taking Ibuprofen 3 – 4 times daily.
Since Mary's pain is moderate, you evaluate your options of drugs for moderate to severe pain.


Self Quiz
Ask yourself...
- How do you assess and evaluate a patient's pain level?
- What are the different types of pain and their management strategies?
- How do you determine the appropriate dosage of pain medications for a patient?
- How do you assess the effectiveness of pain medications in your patients?
- How do you adjust medication dosages for elderly patients with pain or addiction?
- How do you address the unique challenges in pain management for pediatric patients?
- What is the role of non-pharmacological interventions in pain management?
- How do you incorporate non-pharmacological interventions into your treatment plans?
Opioid Classifications and Drug Schedules
A comprehensive understanding of drug schedules and opioid classifications is essential for nurse practitioners to ensure patient safety, prevent drug misuse, and adhere to legal and regulatory requirements. Nurse practitioners with a comprehensive understanding of drug schedules and opioid classifications can effectively communicate with colleagues, ensuring accurate medication reconciliation and facilitating interdisciplinary care. Nurse practitioners’ knowledge in facilitating discussions with pharmacists regarding opioid dosing, potential interactions, and patient education is essential (49).
Drug scheduling became mandated under the Controlled Substance Act. The Drug Enforcement Agency (DEA) Schedule of Controlled Drugs and the criteria and common drugs are listed below.
|
Schedule |
Criteria | Examples |
|
I |
No medical use; high addiction potential |
Heroin, marijuana, PCP |
|
II |
Medical use; high addiction potential |
Morphine, oxycodone, Methadone, Fentanyl, amphetamines |
|
III |
Medical use; high addiction potential |
Hydrocodone, codeine, anabolic steroids |
|
IV |
Medical use, low abuse potential |
Benzodiazepines, meprobamate, butorphanol, pentazocine, propoxyphene |
| V | Medical use; low abuse potential |
Buprex, Phenergan with codeine |
(Pain Physician, 2008)
Listed below are drugs classified by their schedule and mechanism of action. "Agonist" indicates a drug that binds to the opioid receptor, causing pain relief and also euphoria. An agonist-antagonist indicates the drug binds to some opioid receptors but blocks others. Mixed antagonist-agonist drugs control pain but have a lower potential for abuse and dependence than agonists (7).
| Schedule I | Schedule II | Schedule III | Schedule IV | Schedule V | |
| Opioid agonists |
BenzomorphineDihydromor-phone, Ketobemidine, Levomoramide, Morphine-methylsulfate, Nicocodeine, Nicomorphine, Racemoramide |
Codeine, Fentanyl, Sublimaze, Hydrocodone, Hydromorphone, Dilaudid, Meperidine, Demerol, Methadone, Morphine, Oxycodone, Endocet, Oxycontin, Percocet, Oxymorphone, Numorphan |
Buprenorphine Buprenex, Subutex, Codeine compounds, Tylenol #3, Hydrocodone compounds, Lortab, Lorcet, Tussionex, Vicodin |
Propoxyphene, Darvon, Darvocet | Opium, Donnagel, Kapectolin |
| Mixed Agonist -Antagonist | BuprenorphineNaloxone, Suboxone |
Pentazocine, Naloxone, Talwin-Nx |
|||
| Stimulants | N-methylampheta-mine 3, 4-methylenedioxy amphetamine, MDMA, Ecstacy | Amphetamine, Adderal, Cocaine, Dextroamphetamine, Dexedrine, Methamphetamine, Desoxyn, Methylphenidate, Concerta, Metadate, Ritalin, Phenmetrazine, Fastin, Preludin | Benapheta-mine, Didrex, Pemolin, Cylert, Phendimetra-zine, Plegine | Diethylpropion, Tenuate, Fenfluramine, Phentermine Fastin | 1-dioxy-ephedrine-Vicks Inhaler |
| Hallucinogen-gens, other | Lysergic Acid Diamine LSD, marijuana, Mescaline, Peyote, Phencyclidine PCP, Psilocybin, Tetrahydro-cannabinol | Dronabinol, Marinol | |||
| Sedative Hypnotics |
Methylqualine, Quaalude, Gamma-hydroxy butyrate, GHB
|
Amobarbitol, Amytal, Glutethamide, Doriden, Pentobarbital, Nembutal, Secobarbital, Seconal |
Butibarbital. Butisol, Butilbital, Florecet, Florinal, Methylprylon, Noludar |
Alprazolam, Xanax, Chlordiazepoxide, Librium, Chloral betaine, Chloral hydrate, Noctec, Chlorazepam, Clonazepam, Klonopin, Clorazopate, Tranxene, Diazepam, Valium, Estazolam, Prosom, Ethchlorvynol, Placidyl, Ethinamate, Flurazepam, Dalmane, Halazepam, Paxipam, Lorazepam, Ativan, Mazindol, Sanorex, Mephobarbital, Mebaral, Meprobamate, Equanil, Methohexital, Brevital Sodium, Methyl-phenobarbital, Midazolam, Versed, Oxazepam, Serax, Paraldehyde, Paral, Phenobarbital, Luminal, Prazepam, Centrax, Temazepam, Restoril, Triazolam, Halcion, Sonata, Zolpidem, Ambien |
Diphenoxylate preparations, Lomotil |
(41).

Self Quiz
Ask yourself...
- What are the potential risks and benefits of using opioids for pain management?
- How can nurse practitioners effectively monitor patients on long-term opioid therapy?
- What are the potential risks and benefits of using long-acting opioids for chronic pain?
- How do you monitor patients on long-acting opioids for safety and efficacy?
Commonly Prescribed Opioids, Indications for Use, and Typical Side Effects
Opioid medications are widely used for managing moderate to severe pain. Referencing NIDA (2023), this section aims to give healthcare professionals an overview of the indications and typical side effects of commonly prescribed Schedule II opioid medications, including hydrocodone, oxycodone, morphine, Fentanyl, and hydromorphone.
Opioids are derived and manufactured in several ways. Naturally occurring opioids come directly from the opium poppy plant. Synthetic opioids are manufactured by chemically synthesizing compounds that mimic the effects of a natural opioid. Semi-synthetic is a mix of naturally occurring and man-made (35).
Understanding the variations in how an opioid is derived and manufactured is crucial in deciding the type of opioid prescribed, as potency and analgesic effects differ. Synthetic opioids are often more potent than naturally occurring opioids. Synthetic opioids have a longer half-life and slower elimination, affecting the duration of action and timing for dose adjustments. They are also associated with a higher risk of abuse and addiction (38).
Hydrocodone
Mechanism of Action and Metabolism
Hydrocodone is a Schedule II medication. It is an opioid agonist and works as an analgesic by activating mu and kappa opioid receptors located in the central nervous system and the enteric plexus of the bowel. Agonist stimulation of the opioid receptors inhibits nociceptive neurotransmitters' release and reduces neuronal excitability (17).
- Produces analgesia.
- Suppresses the cough reflex at the medulla.
- Causes respiratory depression at higher doses.
Hydrocodone is indicated for treating severe pain after nonopioid therapy has failed. It is also indicated as an antitussive for nonproductive cough in adults over 18.
Available Forms
Hydrocodone immediate release (IR) reaches maximum serum concentrations in one hour with a half-life of 4 hours. Extended-release (ER) Hydrocodone reaches peak concentration at 14-16 hours and a half-life of 7 to 9 hours. Hydrocodone is metabolized to an inactive metabolite in the liver by cytochrome P450 enzymes CYP2D6 and CYP3A4. Hydrocodone is converted to hydromorphone and is excreted renally. Plasma concentrations of hydromorphone are correlated with analgesic effects rather than hydrocodone.
Hydrocodone is formulated for oral administration into tablets, capsules, and oral solutions. Capsules and tablets should never be crushed, chewed, or dissolved. These actions convert the extended-release dose into immediate release, resulting in uncontrolled and rapid release of opioids and possible overdose.
Dosing and Monitoring
Hydrocodone IR is combined with acetaminophen or ibuprofen. The dosage range is 2.5mg to 10mg every 4 to 6 hours. If formulated with acetaminophen, the dosage is limited to 4gm/day.
Hydrocodone ER is available as tablets and capsules. Depending on the product, the dose of hydrocodone ER formulations in opioid-naïve patients is 10 to 20 mg every 12 to 24 hours.
Nurse practitioners should ensure patients discontinue all other opioids when starting the extended-release formula.
Side Effects and Contraindications
Because mu and kappa opioid receptors are in the central nervous system and enteric plexus of the bowel, the most common side effects of hydrocodone are constipation and nausea (>10%).
Other adverse effects of hydrocodone include:
- Respiratory: severe respiratory depression, shortness of breath
- Cardiovascular: hypotension, bradycardia, peripheral edema
- Neurologic: Headache, chills, anxiety, sedation, insomnia, dizziness, drowsiness, fatigue
- Dermatologic: Pruritus, diaphoresis, rash
- Gastrointestinal: Vomiting, dyspepsia, gastroenteritis, abdominal pain
- Genitourinary: Urinary tract infection, urinary retention
- Otic: Tinnitus, sensorineural hearing loss
- Endocrine: Secondary adrenal insufficiency (17)
Hydrocodone, being an agonist, must not be taken with other central nervous system depressants as sedation and respiratory depression can result. In formulations combined with acetaminophen, hydrocodone can increase the international normalized ratio (INR) and cause bleeding. Medications that induce or inhibit cytochrome enzymes can lead to wide variations in absorption.
The most common drug interactions are listed below:
- Alcohol
- Benzodiazepines
- Barbiturates
- other opioids
- rifampin
- phenytoin
- carbamazepine
- cimetidine,
- fluoxetine
- ritonavir
- erythromycin
- diltiazem
- ketoconazole
- verapamil
- Phenytoin
- John’s Wort
- Glucocorticoids
Considerations
Use with caution in the following:
- Patients with Hepatic Impairment: Initiate 50% of the usual dose
- Patients with Renal Impairment: Initiate 50% of the usual dose
- Pregnancy: While not contraindicated, the FDA issued a black-boxed warning since opioids cross the placenta, and prolonged use during pregnancy may cause neonatal opioid withdrawal syndrome (NOWS).
- Breastfeeding: Infants are susceptible to low dosages of opioids. Non-opioid analgesics are preferred.
Pharmacogenomic: Genetic variants in hydrocodone metabolism include ultra-rapid, extensive, and poor metabolizer phenotypes. After administration of hydrocodone, hydromorphone levels in rapid metabolizers are significantly higher than in poor metabolizers.
Oxycodone
Mechanism of Action and Metabolism
Oxycodone has been in use since 1917 and is derived from Thebaine. It is a semi-synthetic opioid analgesic that works by binding to mu-opioid receptors in the central nervous system. It primarily acts as an agonist, producing analgesic effects by inhibiting the transmission of pain signals (Altman, Clark, Huddart, & Klein, 2018).
Oxycodone is primarily metabolized in the liver by CYP3A4/5. It is metabolized in the liver to noroxycodone and oxymorphone. The metabolite oxymorphone also has an analgesic effect and does not inhibit CYP3A4/5. Because of this metabolite, oxycodone is more potent than morphine, with fewer side effects and less drug interactions. Approximately 72% of oxycodone is excreted in urine (Altman, Clark, Huddart, & Klein, 2018).
Available Forms
Oxycodone can be administered orally, rectally, intravenously, and as an epidural. For this sake, we will focus on immediate-release and extended-release oral formulations.
- Immediate-release (IR) tablets
- IR capsules
- IR oral solutions
- Extended-release (ER) tablets
Dosing and Monitoring
The dosing of oxycodone should be individualized based on the patient's pain severity, previous opioid exposure, and response. Initial dosages for opioid naïve patients range from 5-15 mg for immediate-release formulations, while extended-release formulations are usually initiated at 10-20 mg. Dosage adjustments may be necessary based on the patient's response, but caution should be exercised. IR and ER formulations reach a steady state at 24 hours and titrating before 24 hours may lead to overdose.
Regular monitoring is essential to assess the patient's response to treatment, including pain relief, side effects, and signs of opioid misuse or addiction. Monitoring should include periodic reassessment of pain intensity, functional status, and adverse effects (Altman, Clark, Huddart, & Klein, 2018).
Side Effects and Contraindications
Common side effects of oxycodone include:
- constipation
- nausea
- sedation
- dizziness
- respiratory depression
- respiratory arrest
- hypotension
- fatal overdose
Oxycodone is contraindicated in patients with known hypersensitivity to opioids, severe respiratory depression, paralytic ileus, or acute or severe bronchial asthma. It should be used cautiously in patients with a history of substance abuse, respiratory conditions, liver or kidney impairment, and those taking other medications that may interact with opioids, such as alcohol (4).
It is also contraindicated with the following medications and classes:
- Antifungal agents
- Antibiotics
- Rifampin
- Carbamazepine
- Fluoxetine
- Paroxetine
Considerations
- Nurse practitioners should consider the variations in the mechanism of action for the following:
- Metabolism differs between males and females: females have been shown to have less concentration of oxymorphone and more CYP3A4/5 metabolites.
- Infants have reduced clearance of oxycodone, increasing side effects.
- Pediatrics have 20-40% increased clearance over adults.
- Reduced clearance with age increases the half-life of oxycodone.
- Pregnant women have a greater clearance and reduced half-life.
- Impairment of the liver reduces clearance.
- Cancer patients with cachexia have increased exposure to oxycodone and its metabolite.
- Maternal and neonate concentrations are similar, indicating placenta crossing (4)
Morphine

Mechanism of Action and Metabolism
Morphine is a naturally occurring opioid alkaloid extracted from the opium poppy. It was isolated in 1805 and is the opioid against which all others are compared. Morphine binds to mu-opioid receptors in the brain and spinal cord, inhibiting the transmission of pain signals and producing analgesia. It is a first-line choice of opioid for moderate to severe acute, postoperative, and cancer-related pain (8).
Morphine undergoes first-pass metabolism in the liver and gut. It is well absorbed and distributed throughout the body. Its main metabolites are morphine-3-glucuronide and morphine-6-glucuronide. Its mean plasma elimination half-life after intravenous administration is about 2 hours. Approximately 90% of morphine is excreted in the urine within 24 hours (8).
Available Forms
Morphine is available in various forms, including.
- immediate-release tablets
- extended release tablets
- oral IR solutions
- injectable solutions
- transdermal patches
Dosing and Monitoring
Morphine is hydrophilic and, as such, has a slow onset time. The advantage of this is that it is unlikely to cause acute respiratory depression even when injected. However, because of the slow onset time, there is more likelihood of morphine overdose due to the ability to “stack” doses in patients experiencing severe pain (Bistas, Lopez-Ojeda, & Ramos-Matos, 2023).
The dosing of morphine depends on the patient's pain severity, previous opioid exposure, and other factors. It is usually initiated at a low dose and titrated upwards as needed. Monitoring pain relief, adverse effects, and signs of opioid toxicity is crucial. Reevaluate benefits and harms with patients within 1 to 4 weeks of starting opioid therapy or of dose escalation. General recommendations for initiating morphine (Bistas, Lopez-Ojeda, & Ramos-Matos, 2023).
Prescribe IR opioids instead of ER opioids.
Prescribe the lowest effective dosage, below 50 Morphine Milligram Equivalents (MME) /day.
Side Effects and Contraindications
Because morphine binds to opioid receptors in the brain and spinal cord, is metabolized in the liver and gut, and has a slow onset, the following side effects are common:
- Constipation
- Nausea
- Vomiting
- Sedation
- Dizziness
- Respiratory depression
- Pruritis
- Sweating
- Dysphoria/Euphoria
- Dry mouth
- Anorexia
- Spasms of urinary and biliary tract
Contraindications of morphine are:
- Known hypersensitivity or allergy to morphine.
- Bronchial asthma or upper airway obstruction
- Respiratory depression in the absence of resuscitative equipment
- Paralytic ileus
- Risk of choking in patients with dysphagia, including infants, children, and the elderly (8)
Concurrent use with other sedating medications: Amitriptyline, diazepam, haloperidol, chlorpromazine
Morphine interacts with the following medications:
- Ciprofloxacin
- Metoclopramide
- Ritonavir
Considerations for Nurse Practitioners
Assess for medical conditions that may pose serious and life-threatening risks with opioid use, such as the following:
- Sleep-disordered breathing, such as sleep apnea.
- Pregnancy
- Renal or hepatic insufficiency
- Age >= 65
- Certain mental health conditions
- Substance use disorder
- Previous nonfatal overdose
Fentanyl
Mechanism of Action and Metabolism
Fentanyl is a synthetic opioid more potent than morphine and was approved in 1968. Fentanyl is an agonist that works by binding to the mu-opioid receptors in the central nervous system. This binding inhibits the transmission of pain signals, resulting in analgesia. Fentanyl is often used for severe pain management, particularly in the perioperative and palliative care settings, or for severe pain in patients with Hepatic failure (8).
It is a mu-selective opioid agonist. However, it can activate other opioid receptors in the body, such as the delta and kappa receptors, producing analgesia. It also activates the Dopamine center of the brain, stimulating relaxation and exhilaration, which is responsible for its high potential for addiction (8).
Indications for fentanyl are as follows:
- Preoperative analgesia
- Anesthesia adjunct
- Regional anesthesia adjunct
- General anesthesia
- Postoperative pain control
- Moderate to severe acute pain (off-label)
Available Forms
- Fentanyl is available in various forms, including:
- transdermal patches
- injectable solutions
- lozenges
- nasal sprays
- oral tablets (8)
Dosing and Monitoring
Fentanyl is metabolized via the CYP3A4 enzyme in the liver. It has a half-life of 3 to 7 hours, and 75% of Fentanyl is excreted in the urine and 9% in feces.
The dosing of fentanyl depends on the route of administration and the patient's needs. For example, transdermal patches are typically applied every 72 hours, while injectable solutions are titrated to achieve the desired analgesic effect. Monitoring should include assessing pain levels, respiratory rate, blood pressure, and sedation scores (8).
Fentanyl is most dosed as follows:
- Post-operative pain control
- 50 to 100 mcg IV/IM every 1 to 2 hours as needed; alternately 0.5 to 1.5 mcg/kg/hour IV as needed. Consider lower dosing in patients 65 and older.
PCA (patient-controlled analgesia): 10 to 20 mcg IV every 6 to 20 minutes as needed; start at the lowest effective dose for the shortest effective duration - refer to institutional protocols (8).
Moderate to severe acute pain (off-label) 1 to 2 mcg/kg/dose intranasally each hour as needed; the maximum dose is 100 mcg. Use the lowest effective dose for the shortest effective duration (8).
Side Effects and Contraindications
Common side effects of fentanyl include:
- respiratory depression
- sedation
- constipation
- nausea
- vomiting
- euphoria
- confusion
- respiratory depression/arrest
- visual disturbances
- dyskinesia
- hallucinations
- delirium
- narcotic ileus
- muscle rigidity
- addiction
- loss of consciousness
- hypotension
- coma
- death (8).
The use of fentanyl is contraindicated in patients in the following situations:
- After operative interventions in the biliary tract, these may slow hepatic elimination of the drug.
- With respiratory depression or obstructive airway diseases (i.e., asthma, COPD, obstructive sleep apnea, obesity hyperventilation, also known as Pickwickian syndrome)
- With liver failure
- With known intolerance to fentanyl or other morphine-like drugs, including codeine or any components in the formulation.
- With known hypersensitivity (i.e., anaphylaxis) or any common drug delivery excipients (i.e., sodium chloride, sodium hydroxide) (8).
Considerations for Nurse Practitioners
Nurse practitioners prescribing fentanyl should thoroughly assess the patient's pain, medical history, and potential risk factors for opioid misuse. They should also educate patients about the proper use, storage, and disposal of fentanyl. It should be used cautiously in patients with respiratory disorders, liver or kidney impairment, or a history of substance abuse. Fentanyl is contraindicated in patients with known hypersensitivity to opioids and those without exposure to opioids.
Alcohol and other drugs, legal or illegal, can exacerbate fentanyl's side effects, creating multi-layered clinical scenarios that can be complex to manage. These substances, taken together, generate undesirable conditions that complicate the patient's prognosis (8).
Hydromorphone
Mechanism of Action and Metabolism
Hydromorphone is a semi-synthetic opioid derived from morphine. It binds to the mu-opioid receptors in the central nervous system. It primarily exerts its analgesic effects by inhibiting the release of neurotransmitters involved in pain transmission, thereby reducing pain perception. Hydromorphone also exerts its effects centrally at the medulla level, leading to respiratory depression and cough suppression (1).
Hydromorphone is indicated for:
- moderate to severe acute pain
- severe chronic pain
- refractory cough suppression (off-label) (1)
Available Forms
Hydromorphone is available in various forms, depending on the patient’s needs and severity of pain.
- immediate-release tablet
- extended release tablets
- oral liquid
- injectable solution
- rectal suppositories
Dosing and Monitoring
The immediate-release oral formulations of hydromorphone have an onset of action within 15 to 30 minutes. Peak levels are typically between 30 and 60 minutes with a half-life of 2 to 3 hours. Hydromorphone is primarily excreted through the urine.
The dosing of hydromorphone should be individualized based on the patient's pain intensity, initiated at the lowest effective dose, and adjusted gradually as needed. Close monitoring of pain relief, adverse effects, and signs of opioid toxicity is essential. Patients should be assessed regularly to ensure they receive adequate pain control without experiencing excessive sedation or respiratory depression.
The following are standard dosages that should only be administered when other opioid and non-opioid options fail.
- Immediate-release oral solutions dosage: 1 mg/1 mLoral tablets are available in 2 mg, 4 mg, and 8 mg.
- Extended-release oral tablets are available in dosages of 8 mg, 12 mg, 16 mg, and 32 mg.
- Injection solutions are available in concentrations of 1 mg/mL, 2 mg/mL, 4 mg/mL, and 10 mg/mL.
- Intravenous solutions are available in strengths of 2 mg/1 mL, 2500 mg/250 mL, ten mg/1 mL, and 500 mg/50 mL.
- Suppositories are formulated at a strength of 3 mg (1).
Side Effects and Contraindications
Hydromorphone has potential adverse effects on several organ systems, including the integumentary, gastrointestinal, neurologic, cardiovascular, endocrine, and respiratory.
Common side effects of hydromorphone include:
- Constipation
- Nausea
- Vomiting
- Dizziness
- Sedation
- respiratory depression
- pruritus
- headache
- Somnolence
- Severe adverse effects of hydromorphone include:
- Hypotension
- Syncope
- adrenal insufficiency
- coma
- raised intracranial pressure.
- seizure
- suicidal thoughts
- apnea
- respiratory depression or arrest
- drug dependence or withdrawal
- neonatal drug withdrawal syndrome
- Hydromorphone is contraindicated in patients with:
- known allergies to the drug, sulfites, or other components of the formulation.
- known hypersensitivity to opioids.
- severe respiratory depression
- paralytic ileus
- acute or severe bronchial asthma (1).
Caution should be exercised in patients with:
- respiratory insufficiency
- head injuries
- increased intracranial pressure.
- liver or kidney impairment.
Considerations for Nurse Practitioners
As nurse practitioners, it is crucial to assess the patient's pain intensity and overall health status before initiating Hydromorphone. Start with the lowest effective dose and titrate carefully for optimal pain control. Regular monitoring for adverse effects, signs of opioid toxicity, and therapeutic response is essential. Educate patients about the potential side effects, proper dosing, and the importance of not exceeding prescribed doses. Additionally, nurse practitioners should be familiar with local regulations and guidelines regarding opioid prescribing and follow appropriate documentation and monitoring practices.
Additional Considerations
In terminal cancer patients, clinicians should not restrain opioid therapy even if signs of respiratory depression become apparent.
Hydromorphone requires careful administration in cases of concurrent psychiatric illness.
Specific Patient Considerations:
- Hepatic impairment and Renal Impairment: Initiate hydromorphone treatment at one-fourth to one-half of the standard starting dosage, depending on the degree of impairment.
- Pregnancy considerations: Hydromorphone can traverse the placental barrier and induce NOWS.
- Breastfeeding considerations: Nonopioid analgesic agents are preferable for breastfeeding women.
- Older patients: hydromorphone is categorized as a potentially inappropriate medication for older adults (1).
Tramadol

Mechanism of Action and Metabolism
Tramadol is a Schedule IV opioid medication with a higher potential for dependency and misuse than non-opioid medications. It binds to opioid receptors in the central nervous system, inhibiting the reuptake of norepinephrine and serotonin. It also has weak mu-opioid receptor agonist activity.
The liver metabolizes tramadol mediated by the cytochrome P450 pathways (particularly CYP2D6) and is mainly excreted through the kidneys.
Tramadol is used for moderate to severe pain.
Available Forms of Tramadol include:
- Immediate-release-typically used for acute pain management.
- Extended-release-used for chronic pain.
Dosing and Monitoring
Tramadol has an oral bioavailability of 68% after a single dose and 90–100% after multiple doses and reaches peak concentrations within 2 hours. Approximately 75% of an oral dose is absorbed, and the half-life of tramadol is 9 hours (18).
Tramadol dosing should be individualized based on the patient's pain severity and response.
The initial dose for adults is usually 50-100 mg orally every 4-6 hours for pain relief. The maximum daily dose is 400 mg for immediate-release formulations and 300 mg for extended-release formulations (18).
It is essential to monitor the patient's pain intensity, response to treatment, and any adverse effects. Regular reassessment and adjustment of the dosage may be necessary.
Side Effects and Contraindications
Tramadol is responsible for severe intoxications leading to consciousness disorder (30%), seizures (15%), agitation (10%), and respiratory depression (5%). The reactions to Tramadol suggest that the decision to prescribe should be carefully considered.
Common Side Effects of Tramadol Include:
- Nausea
- Vomiting
- Dizziness
- Constipation
- Sedation
- Headache
- CNS depression
- Seizure
- Agitation
- Tachycardia
- Hypertension
- reduced appetite
- pruritus and rash
- gastric irritation
Serious side effects include:
- respiratory depression
- serotonin syndrome
- seizures
Contraindications
Tramadol is contraindicated in patients with:
- history of hypersensitivity to opioids
- acute intoxication with alcohol
- opioids, or other psychoactive substances
- Patients who have recently received monoamine oxidase inhibitors (MAOIs)
Additionally, the following can be observed in tramadol intoxication:
- miosis
- respiratory depression
- decreased level of consciousness
- hypertension
- tremor
- irritability
- increased deep tendon reflexes
Poisoning leads to:
- multiple organ failure
- coma
- cardiopulmonary arrest
- death
Considerations for Nurse Practitioners
Tramadol has been increasingly misused with intentional overdoses or intoxications. Suicide attempts were the most common cause of intoxication (52–80%), followed by abuse (18–31%), and unintentional intoxication (1–11%). Chronic tramadol or opioid abuse was reported in 20% of tramadol poisoning cases. Fatal tramadol intoxications are uncommon except when ingested concurrent with depressants, most commonly benzodiazepines and alcohol (18).
Tramadol poisoning can affect multiple organ systems:
- gastrointestinal
- central nervous system: seizure, CNS depression, low-grade coma, anxiety, and over time anoxic brain damage
- Cardiovascular system: palpitation, mild hypertension to life-threatening complications such as cardiopulmonary arrest
- respiratory system
- renal system: renal failure with higher doses of tramadol intoxication
- musculoskeletal system: rhabdomyolysis
- endocrine system: hypoglycemia, serotonin syndrome (18)
Cannabis
Mechanism of Action and Metabolism
Cannabis is classified as a Schedule I status. It contains various cannabinoids, with delta-9-tetrahydrocannabinol (THC) and cannabidiol (CBD) being the most studied. THC primarily acts on cannabinoid receptors in the brain, producing psychoactive effects, while CBD has more diverse effects on the nervous system. These cannabinoids interact with the endocannabinoid system, modulating neurotransmitter release and influencing various physiological processes (32).
Similar to opioids, cannabinoids are synthesized and released in the body by synapses that act on the cannabinoid receptors present in presynaptic endings (32). They perform the following actions related to analgesia:
- Decrease the release of neurotransmitters.
- Activate descending inhibitory pain pathways.
- Reduce postsynaptic sensitivity and alleviate neural inflammation.
- Modulate CB1 receptors within central nociception processing areas and the spinal cord, resulting in analgesic effects.
- Attenuate inflammation by activating CB2 receptors (32).
- Emerging research shows cannabis is indicated for:
- Migraines
- chronic pain
- back pain
- arthritic pain
- pain associated with cancer and surgery.
- neuropathic pain
- diabetic neuropathic pain when administered early in the disease progression.
- sickle cell disease
- cancer
- inflammatory bowel disease (32)
Available Forms
Cannabis refers to products sourced from the Cannabis sativa plant. There are differences between cannabis, cannabinoids, and cannabidiol (CBD). Cannabinoids are extracted from the cannabis plants. Cannabinoid-based treatments, such as dronabinol and CBD, are typically approved medical interventions for specific indications. THC (9-tetrahydrocannabinol) is the psychoactive component of the cannabis plant. CBD is a non-psychoactive component (32).
Cannabis can be consumed in different forms, each with a different onset and duration. Patients may have individual preferences, including:
- smoking/vaporizing dried flowers.
- consuming edibles
- tinctures or oils
- applying topicals (32)
Dosing and Monitoring
Inhaling marijuana via the lungs by smoking or vaping causes maximum plasma concentration within minutes. Psychiatric effects begin within seconds to a few minutes after inhalation and peak after 15 to 30 minutes. The effect diminishes throughout 2 to 3 hours (32).
Oral ingestion of marijuana causes psychiatric effects that typically occur between 30 and 90 minutes and reach maximum effect after 2 to 3 hours. Ingested marijuana effects last about 4 to 12 hours (32).
Dosing cannabis is challenging due to variations in potency and individual responses. Start with low doses and titrate slowly to achieve the desired effect while minimizing side effects. Regular monitoring is crucial, including assessing symptom relief, adverse effects, and potential drug interactions. Encourage patients to keep a diary to track their cannabis use and its effects (32).
Side Effects and Contraindications
Cannabis can exacerbate mental health conditions such as anxiety and psychosis. Common side effects of cannabis include (32):
- Dizziness
- dry mouth
- increased heart rate
- impaired memory
- psychoactive effects
Contraindications include:
- Pregnancy
- Breastfeeding
- heart disease
- respiratory conditions
- history of substance abuse
- mental health disorders

Self Quiz
Ask yourself...
- How do you address patients' misconceptions about pain medications?
- What are the mechanisms of action for commonly prescribed pain medications?
- How do these mechanisms of action contribute to pain relief?
- What are the potential side effects and risks associated with commonly prescribed pain medications?
- How do you educate patients about the risks and benefits of pain medications?
- How do you manage patients who require high-dose opioids for pain management?
- Is medical cannabis legal in your State? If yes, are you familiar with the prescribing guidelines?
- Do you have any personal biases against the use of medical cannabis? Why or why not?
Case Study
Mary is agreeable to trying an increased dose of Gabapentin. Mary would also like to see a counselor to discuss her past and get help with her anxiety. You made an appointment for Mary to see a Licensed Clinical Social Worker in your clinic.
You read the side effects and warnings for Gabapentin, and it is unsafe to use Gabapentin and Tramadol together since they are both depressants. You order a non-steroidal drug for Mary's somatic knee pain and make a consult for imaging studies on her left knee. You also make a referral to Orthopedics.
You educated Mary about the side effects of Gabapentin and scheduled a follow-up appointment. The day after Mary began her treatment with the increased Gabapentin, you called Mary to follow up on its effect. Mary still has pain, but she is not having any untoward side effects. Gabapentin may not work immediately so you will schedule a follow-up call in 3 days.


Self Quiz
Ask yourself...
- In this case study, Mary has insurance. How might your practice be different were Mary not insured?
- In your experience, what are the possible reasons for Mary's knee pain not being a part of her previous treatment record?
- Consider how your assessment of Mary's needs differs from the above-mentioned case study.
- Explain the rationale for decisions made by the nurse practitioner in the case study mentioned above and if your decisions would differ.
Opioid Use, the Opioid Epidemic, and Statistics
The use and misuse of opioids has become a pressing public health concern, leading to a global epidemic. The history of opioid use, the opioid epidemic, and associated statistics provide essential context for healthcare professionals in addressing this public health crisis. More importantly, it is estimated that 1 in 4 patients receiving prescription opioids in primary care settings will misuse them. In addition, 50% of opioid prescriptions are written by primary care providers, including nurse practitioners (22). Understanding the factors contributing to the epidemic and the magnitude of its impact is crucial for effective prevention, intervention, and treatment strategies.
History of Opioid Use
Opioids have a long history of medicinal use, dating back to ancient civilizations. They have been a drug of choice for pain relief for thousands of years. The introduction of synthetic opioids in the 19th century, such as morphine and later heroin, revolutionized pain management. However, their potential for addiction and misuse soon became apparent (16).
The Opioid Epidemic
The opioid epidemic refers to the surge in opioid misuse, addiction, and overdose deaths. The epidemic gained momentum in the late 1990s with increased prescribing of opioids for chronic pain (43).
No doubt, increased prescribing put opioids in the hands of consumers, but increased prescribing resulted from a multifactorial influence. One of the main influences was aggressive marketing by pharmaceutical companies, which has been well publicized. However, due to the long history of underprescribing pain medications for fear of misuse and addiction, the medical community was primed to expand its opioid prescribing practices (31).
A historical event that increased comfort with prescribing opioids, in the writer's opinion, was the introduction of the Medicare Hospice Benefit in 1986. Medical directors must be contracted or employed by hospices, and these medical directors had or soon gained pain management expertise. To further promote hospice and effective pain management, the hospice medical directors, with newly acquired skills, provided education throughout medical communities about pain management and specifically to decrease the fear of using opioids. Pharmacies and attending physicians grew accustomed to giving opioids for home use. Hospice care is for terminally ill patients, defined as a life expectancy of 6 months or less. Still, the reality is that hospice discharges 12 to 40% of patients for ineligibility and other reasons.
A more prominent factor in increasing opioid prescribing was the 1996 American Pain Society's introduction of pain as "the 5th Vital sign." Soon after, The Joint Commission promoted pain as "the 5th Vital Sign" and began compliance surveys in healthcare organizations requiring pain assessment details to be as prominent as blood pressure and heart rate. The Joint Commission cited a quote from 1968 by a nurse from the University of California Los Angeles, Margo McCaffrey, who defined pain as "…Whatever the experiencing person says it is, existing whenever s/he says it does." The Joint Commission accreditation programs pursued pain management as part of the accreditation process throughout its healthcare accreditation programs, including hospice accreditation by 1989 per TJC Timeline (48).
The National Institute of Health published an article about the Joint Commission's role in the opioid epidemic, particularly regarding the definition of pain, "This definition emphasizes that pain is a subjective experience with no objective measures. It also stresses that the patient, not the clinician, is the authority on the pain and that their self-report is the most reliable indicator of pain. This set the tone for clinicians: Patients are always to be trusted to report pain accurately” (45).
Statistics on the Opioid Epidemic
In the United States alone, over 500,000 people died from opioid overdoses between 1999 and 2017. The number of opioid-related overdose deaths continues to increase, with synthetic opioids, mainly illicitly manufactured Fentanyl, playing a significant role in recent years (46). Fentanyl-laced drugs, such as marijuana, are increasingly sold knowing and unknowingly to introduce medications with a high addiction rate, thus creating new consumers. This practice can potentially increase deaths due to the imprecise nature of manufacturing (16).
Opioid-related hospitalizations have also risen substantially. In 2014, there were approximately 1.27 million hospitalizations related to opioids in the United States. These hospitalizations not only place a burden on healthcare systems but also reflect the severe consequences of opioid misuse (3).


Self Quiz
Ask yourself...
- Have you experienced changes to your practice because of the opioid epidemic? If so, what are the changes?
- What is your opinion on the validity of Margo McCaffrey's definition of pain?
- What factors influence your willingness or unwillingness to prescribe opioids?
Federal Regulations on Opioid Prescribing
The history of substance use disorder prevention that promotes opioid recovery and treatment for patients and communities can be traced back to the early 20th century. However, the current approach to addressing opioid addiction and promoting healing has evolved significantly in recent times (36).
In the early 1900s, health professionals treated opioid addiction with punitive measures, including incarceration and moralistic approaches. The focus was on punishing individuals rather than providing effective treatment. This approach persisted for several decades until the mid-20th century when the medical community started recognizing addiction as a medical condition rather than a moral failing (36).
The Controlled Substances Act (CSA), introduced in 1970, was a response to increasing drug abuse and illicit drug trafficking in the United States. The CSA is a federal law regulating the manufacture, possession, distribution, and use of certain substances, including drugs and medications, that can potentially cause abuse and dependence. Its primary purpose is to combat drug abuse, reduce drug-related crimes, and protect public health and safety. The Drug Enforcement Agency (DEA) plays a crucial role in enforcing the CSA by monitoring and controlling controlled substance production, distribution, and use (31).
In the 1990s, the significant increase in opioid prescribing, leading to a surge in opioid addiction and overdose deaths, prompted a shift in focus toward prevention. Efforts were made to educate healthcare providers about the risks of overprescribing opioids and to implement prescription drug monitoring programs to track and prevent abuse (36).
The Comprehensive Addiction and Recovery Act (CARA) was signed into law in 2016 to expand access to treatment and recovery services for opioid addiction. This legislation allocated funding for prevention, treatment, recovery, and support services while promoting evidence-based practices and programs (36).
The Centers for Disease Control and Prevention (CDC) published guidelines in 2016 for prescribing opioids for chronic pain, which was updated in 2022. These guidelines emphasize the importance of non-opioid alternatives, using the lowest effective dose for the shortest duration, and assessing the benefits and risks of continued opioid therapy (13).
Furthermore, the Substance Use Disorder Prevention that Promotes Opioid Recovery and Treatment for Patients and Communities Act (SUPPORT) was signed into law in 2018, providing additional resources to address the opioid crisis. This legislation expanded access to medication-assisted treatment (MAT), increased the availability of naloxone, a medication used to reverse opioid overdose, and enhanced support for recovery housing (36).
In recent years, there has been a growing recognition of the importance of a comprehensive approach to opioid addiction, including harm reduction strategies, increased access to naloxone, and the integration of mental health services. Communities and organizations have been working together to address the underlying issues contributing to addiction, such as poverty, trauma, and social determinants of health (50).
Overall, the history of substance use disorder prevention that promotes opioid recovery and treatment has evolved from a punitive approach to a more compassionate and evidence-based model. Efforts are now focused on prevention, early intervention, and expanding access to comprehensive treatment and support services for individuals and communities affected by opioid addiction (36).
The most current federal regulations on opioid prescribing for healthcare providers are the amendments to the CSA in 2018, which added new rules to limit the quantity and duration of opioid prescriptions for acute pain to seven days. In 2022, the CDC updated recommendations to the Clinical Practice Guidelines for Prescribing Opioids for Pain.
The 2022 CDC guidelines are summarized below (13):
- Non-opioid therapies should be considered the first-line treatment for chronic pain.
- Establish clear treatment goals with patients, including realistic pain management and functional improvement expectations.
- Conduct a thorough risk assessment for potential harms before initiating opioid therapy.
- When opioids are used, start with the lowest effective dose and consider immediate-release opioids instead of extended-release or long-acting opioids.
- Prescribe the lowest effective dose for the shortest duration possible, typically three days or less and rarely exceeding seven days.
- Reassess benefits and risks within one day after prescribing opioids, including checking the prescription drug monitoring database.
- Avoid prescribing opioids and benzodiazepines concurrently whenever possible due to the increased risk of overdose and death.
- Offer naloxone to patients at increased risk of opioid overdose, including those with a history of overdose, substance use disorder, or concurrent benzodiazepine use.
- When opioids are no longer needed, taper the dose gradually to minimize withdrawal symptoms.
- Arrange an evidence-based treatment for patients with opioid use disorder, including medication-assisted treatment (Naltrexone, Buprenorphine, or Methadone).

Self Quiz
Ask yourself...
- What are the guidelines general for prescribing opioids for acute pain?
- How do these guidelines differ for chronic pain management?
- Discuss how federal regulations impact the practice of nurse practitioners in terms of opioid prescribing.
- Describe the potential benefits and challenges nurse practitioners face when adhering to federal regulations on opioid prescribing.
- How can nurse practitioners navigate and stay updated with evolving federal regulations surrounding opioid prescribing to ensure safe and effective care?
- How do you ensure appropriate documentation when prescribing controlled substances?
Safe Prescribing and Prescription Monitoring Program
Prescription Drug Monitoring Programs (PDMP) are state-run electronic databases that track.
the prescribing and dispensing of controlled substances. PDMPs are designed to improve patients.
care and safety by giving clinicians access to patients' prescription histories, allowing them to make informed decisions when prescribing controlled substances. PDMPs help identify patients at risk of substance misuse or prescription drug overdose. They also enable clinicians to identify potential drug interactions and prevent opioid diversion (14).
PDMPs collect and store data from pharmacies and prescribers in a centralized database. Clinicians can access this database to review a patient's prescription history, including the types of medications prescribed, the prescribers involved, and the dispensing pharmacies (14).
In many states, PDMP use is mandated by law, and nurse practitioners may be required to register and use the system. It is essential to understand state-specific laws and regulations regarding PDMP use.
PDMPs have some limitations, such as incomplete data or delays in reporting. The CDC emphasizes that clinicians should use PDMP data for their clinical assessment and other relevant information to make informed decisions about prescribing controlled substances. Still, PDMP cannot be used as the sole basis for denying or providing treatment (14).
Case Study
After five days on Gabapentin, Mary was doing well, and her neuropathic pain had decreased to 3/10. However, Mary suffered a fall after her knee "gave out" and injured her knee and back. She was in severe pain, and her family drove her to the ER. The ER doctors saw Mary, and orthopedics were consulted. Mary has surgery scheduled for a knee replacement a week from now.
Mary was prescribed Vicodin because she was in excruciating pain, but her prescription only allowed enough medication for two days. Mary has made an appointment with you to renew her prescription.
You evaluate Mary because you know that concomitant use of Gabapentin and opioids puts Mary at risk for respiratory depression and possible side effects, including accidental overdose.
Mary stated she has been more alert the past 24 hours and is afraid her functional status will continue to decline if she does not have more Vicodin because the pain in her back and knee makes it difficult to stand. You assess Mary. Mary stated she occasionally drinks alcohol but has not had a drink since she moved. She has no familial history of substance abuse or mental health disorders.
Mary's mother stayed at her house to help her for the first 24 hours after Mary's return from the ER, but Mary is providing her care now.
You check the PDMP database and see that Mary was prescribed eight pills she has taken over the last 48 hours.
Since the Vicodin has been effective without untoward side effects, and Mary's function is improving, you decide to refill the prescription of Vicodin. You will taper the dose to three Vicodin daily for two days and two for one day. Mary will be near her appointment for a knee replacement as well.


Self Quiz
Ask yourself...
- What are the potential benefits and drawbacks of using PDMPs in your practice?
- How can PDMPs help you identify potential drug abuse or diversion cases among your patients? Can you provide examples from your own experience?
- In what ways do PDMPs impact your decision-making process when prescribing controlled substances?
- What are the key considerations when prescribing controlled substances?
- How do you ensure responsible prescribing practices for controlled substances?
Preventing Opioid Use Disorder
As previously discussed, opioid addiction is a growing concern worldwide, affecting individuals from all walks of life. According to the CDC, "Anyone who takes prescription opioids can become addicted to them" (14).
As frontline healthcare professionals, nurse practitioners must recognize the signs of opioid addiction to provide timely intervention and support. This section will outline the key indicators of opioid addiction.
Physical Symptoms
Physical symptoms are often the first noticeable signs of opioid addiction. These symptoms may include constricted pupils, drowsiness, slurred speech, impaired coordination, and increased sensitivity to pain. Additionally, individuals struggling with opioid addiction may exhibit frequent flu-like symptoms, such as a runny nose, sweating, itching, or gastrointestinal issues.
Behavioral Changes
Opioid addiction can significantly impact an individual's behavior. These may include increased secrecy, frequent requests for early prescription refills, doctor shopping (seeking prescriptions from multiple healthcare providers), neglecting personal hygiene, and experiencing financial difficulties due to excessive spending on opioids (37).

Social Isolation
Opioid addiction often leads to social withdrawal and isolation. Individuals struggling with opioid addiction may distance themselves from family, friends, and social activities they once enjoyed. They may exhibit erratic mood swings, become defensive or hostile when confronted about their drug use, and display a general lack of interest in previously important activities (30).
Psychological Changes
The psychological impact of opioid addiction is significant. Individuals with opioid addiction may exhibit increased anxiety, depression, irritability, and restlessness. They may also experience cognitive impairments, memory lapses, and difficulties in decision-making. Healthcare professionals should be attentive to these changes, as they can indicate opioid addiction (51).
Tolerance and Withdrawal Symptoms
The development of tolerance and withdrawal symptoms are critical signs of opioid addiction. Individuals may require increased dosages of opioids to achieve the desired effect, indicating a growing tolerance. Furthermore, withdrawal symptoms such as muscle aches, nausea, vomiting, insomnia, and intense cravings for opioids may occur when the drug is discontinued or reduced abruptly (51).

Self Quiz
Ask yourself...
- Discuss how nurse practitioners can contribute to preventing opioid use disorder.
- Explain how nurse practitioners effectively communicate the risks and signs of opioid misuse without stigmatizing or alienating patients.
- What are the signs of opioid addiction or misuse in patients?
- How do you approach patients who may be at risk for opioid addiction?
- How do you ensure appropriate documentation when prescribing controlled substances?
Opioid Overdose
The management of opioid overdose, withdrawal, and addiction requires a comprehensive approach that combines pharmacological interventions with psychosocial support. Naloxone remains a vital tool for reversing opioid overdose, while medications such as Methadone, buprenorphine, and naltrexone play crucial roles in withdrawal and addiction treatment (National Institute of Health, 2023). Nurse practitioners must stay vigilant and informed about the evolving landscape of medications. This section aims to provide a comprehensive review of medications and treatment strategies for opioid overdose, withdrawal, and addiction and is excerpted from the NIH (40).
Naloxone
Mechanism of Action and Metabolism
Naloxone is an opioid receptor antagonist. It works by binding to opioid receptors and displacing any opioids present, thereby reversing the effects of opioid overdose. It has a higher affinity for opioid receptors than most opioids, effectively blocking their action.
Naloxone is indicated for emergency intervention of opioid overdose. It effectively reverses respiratory depression and other life-threatening effects. Studies suggest the potential benefits of combining naloxone with other medications, such as buprenorphine (see below), to improve outcomes. Initiatives promoting community-based naloxone distribution programs have shown promising results in reducing opioid-related deaths.
Available Forms
Naloxone is available in various formulations:
- Intranasal
- Intramuscular
- Intravenous
- auto-injectors.
The most used form is the intranasal spray, which is easy to administer and requires no specialized training. Intranasal naloxone formulations have gained popularity due to their ease of use and increased availability. A recent study showed that the non-FDA-approved compound spray was far less effective than either FDA compound (15).
Dosing and Monitoring
The recommended initial dose of naloxone for opioid overdose is 2mg intranasally or 0.4mg to 2mg intramuscularly or intravenously. If the patient does not respond within 23- minutes, additional doses may be administered every 2-3 minutes. Continuous monitoring of the patient's respiratory status is essential, as repeat doses may be required due to the short half-life of naloxone.
Side Effects and Contraindications
Naloxone has been shown not to affect individuals without opioids in their system.
Common side effects of naloxone include
- Withdrawal symptoms: increased heart rate, sweating, and agitation
- nausea
- vomiting
- headache
Contraindications include known hypersensitivity to naloxone and situations where the use of naloxone may be unsafe or not feasible.
Considerations for Nurse Practitioners
Fentanyl and other opioids have a rapid onset, and the need to act quickly is paramount. As mentioned previously, the ease of use and higher plasma concentrations using the FDA-approved 4-mg FDANxSpray device compared with the locally compounded nasal sprays should be considered when ordering Naloxone (15).
Fentanyl and other potent synthetic opioids may require multiple administrations of naloxone to achieve reversal of an overdose (Chiang, Gyaw, & Krieter, 2019). As a nurse practitioner prescribing naloxone, it is crucial to assess the patient's risk factors for opioid overdose, such as a history of substance use disorder or chronic pain management. Education regarding the proper administration of naloxone should be provided to the patients and their caregivers. Additionally, it is essential to provide resources for follow-up care, including addiction treatment and ongoing support.
Methadone
Mechanism of Action and Metabolism
Methadone is a long-acting opioid agonist that effectively suppresses withdrawal symptoms and reduces cravings. It binds to the same opioid receptors in the brain as other opioids. It relieves withdrawal symptoms and reduces cravings by blocking the euphoric effects of opioids, thus helping individuals with opioid dependence to achieve stability (33).
Available Forms
Methadone is available in oral tablets and liquid formulations. The oral tablet is the most used form and is typically administered once daily (33).
Dosing and Monitoring
Methadone dosing is individualized based on the patient's response and needs. Initially, the dose often started low and gradually increased until the patient reached a stable dose. Dosing may need to be adjusted based on the patient's response, adherence, and any changes in their overall health. Regularly monitoring the patient's vital signs, urine drug screens, and assessment of their withdrawal symptoms and cravings is essential.
Side Effects and Contraindications
Common side effects of methadone include:
- Constipation
- dry mouth
- drowsiness
- sweating
- weight gain
- respiratory depression
Contraindications include:
- known hypersensitivity to methadone
- severe asthma
- respiratory depression
- certain heart conditions (33).
Considerations for Nurse Practitioners
As a nurse practitioner prescribing methadone, conducting a comprehensive assessment of the patient's medical history, current medications, and substance use history is crucial. Opioid treatment programs or specialized clinics are often involved in methadone treatment, so collaboration and coordination of care with these programs are essential. Regularly monitoring the patient's progress, adherence, and potential side effects or drug interactions is essential. Additionally, providing education on the risks and benefits of methadone and the importance of adherence to the prescribed regimen is crucial for successful treatment outcomes.
Buprenorphine
Mechanism of Action and Metabolism
Buprenorphine is a partial opioid agonist with a ceiling effect that minimizes the risk of overdose while reducing withdrawal symptoms. Buprenorphine is a partial opioid agonist that binds to the same receptors as other opioids but produces a weaker response. It has a high affinity for the mu-opioid receptors, which helps reduce cravings and withdrawal symptoms in individuals with opioid dependence.
Available Forms
Buprenorphine is available in different formulations, including sublingual tablets, buccal films, and extended-release injections. The sublingual tablets have different strengths, such as 2mg, 4mg, 8mg, and 12mg. Buprenorphine is taken as a daily tablet or weekly or monthly injection.
Dosing and Monitoring
The dosing of buprenorphine varies depending on the individual's opioid dependence severity and treatment phase. Initially, a low dose (e.g., 2-4mg) is given, and it may gradually increase to a maintenance dose of 8-24 mg daily. Regular monitoring is essential to assess the patient's response, adherence, and potential side effects.
Side Effects and Contraindications
Common side effects of buprenorphine include:
- Constipation
- Nausea
- Headache
- Insomnia
- Sweating
Serious side effects are rare but can include:
- Respiratory depression
- Allergic reactions
Buprenorphine is contraindicated in individuals with:
- Severe respiratory insufficiency
- Acute intoxication with opioids
- Known hypersensitivity
Considerations for Nurse Practitioners
Nurse practitioners can prescribe buprenorphine for opioid dependence treatment under the Drug Addiction Treatment Act (DATA). To become eligible, they must complete specific training requirements and obtain a waiver from the Substance Abuse and Mental Health Services Administration (SAMHSA). Nurse practitioners should assess patients thoroughly, including their opioid use history, comorbidities, and medication compatibility, while ensuring appropriate counseling and referral for comprehensive treatment (40).
Clonidine + Lofexidine
Mechanism of Action and Metabolism:
Both Clonidine and Lofexidine are alpha-2 adrenergic agonists. They work by stimulating alpha-2 receptors in the brain, which reduces sympathetic outflow and norepinephrine release. This results in decreased sympathetic activity, leading to various effects such as reduced blood pressure, decreased heart rate, and alleviated withdrawal symptoms (28).
Available Forms
Clonidine is available in oral tablets and patches. Lofexidine is available in oral tablets and is taken as needed (40).
Dosing and Monitoring
For opioid withdrawal, the Clonidine dose ranges from 0.1-0.3 mg every 4-6 hours. Lofexidine is usually initiated at 0.53 mg three times daily, and the dose can be increased to 2.88 mg daily. Monitoring blood pressure and heart rate is essential during treatment (40).
Side Effects and Contraindications:
Common side effects of both medications include:
- dry mouth
- sedation
- dizziness
- constipation
- orthostatic hypotension (40).
Both medications are contraindicated in patients with:
- Hypotension
- Bradycardia
- heart block
- history of hypersensitivity to the drugs (40).
Considerations for Nurse Practitioners:
An early study of lofexidine vs. clonidine for withdrawal symptoms showed that treatment with lofexidine resulted in lower withdrawal symptoms, fewer mood problems, less sedation, and hypotension. There were no significant differences in craving levels, morphine metabolites in urine, or dropout rates when both were compared.
Lofexidine can be a safe option for outpatient treatment as it does not lead to hypotension. However, nurse practitioners must closely monitor patients' blood pressure and heart rate during treatment and educate them about possible side effects. If patients experience any concerning symptoms, they should inform their nurse practitioner immediately.
Gradual dose reduction of Clonidine is crucial to prevent rebound hypertension. Before prescribing either medication, nurse practitioners should assess for any contraindications or potential drug interactions (19).
Emerging Therapies for Withdrawal
Extended-release naltrexone: Naltrexone is an opioid receptor antagonist that blocks the effects of opioids, reducing the risk of relapse. It is taken as a monthly injection.
Alpha-2 adrenergic agonists: Emerging evidence suggests the potential use of dexmedetomidine and guanfacine for managing opioid withdrawal symptoms.
Medication-Assisted Treatment (MAT):
Methadone was introduced in the 1960s and marked a significant turning point in opioid addiction treatment or MAT. Along with counseling and behavioral therapies, MAT became the cornerstone of opioid addiction recovery.
Examples of medications used:
- Methadone
- Buprenorphine:
- Naltrexone:
Adjunctive Pharmacotherapies:
Antidepressants: Selective serotonin reuptake inhibitors and tricyclic antidepressants may help manage co-occurring depression and anxiety.
Anticonvulsants:
Medications like Gabapentin and pregabalin show promise in reducing opioid cravings and improving treatment outcomes.


Self Quiz
Ask yourself...
- What are the mechanisms of action for commonly prescribed addiction medications?
- What are the potential risks and benefits of using benzodiazepines for pain management?
- How do you assess and manage patients with co-occurring pain and substance use disorders?
- What are the guidelines for prescribing addiction medications like buprenorphine or methadone?
- How do these medications work in the treatment of opioid use disorder?
- What are the potential side effects and risks associated with addiction medications?
- How do you support patients in their recovery from opioid use disorder?
- How do you address patients' concerns and fears about addiction medications?
- What are the federal guidelines around prescribing addiction medications for nurse practitioners?
- How do these guidelines influence your prescribing practices?
Other Substance Use Disorders
Patients in pain may struggle with Substance Use Disorders other than Opioid Use Disorder. Substance use disorders may often occur with mental health conditions such as anxiety, depression, and bipolar disorder. In addition, many individuals engage in polydrug use. Understanding the most common Substance Use Disorders aids in a comprehensive assessment of the patient and the development of appropriate treatment plans (28).
Alcohol Use Disorder (AUD):
The prevalence of AUD worldwide was estimated to be 9.8% in men and 5.5% in women in 2016 (28).
Cannabis Use Disorder (CUD):
the prevalence of CUD in the United States increased from 2.18% in 2001-2002 to 2.89% in 2012-2013. (28).
Cocaine Use Disorder:
According to the National Survey on Drug Use and Health (NSDUH), in 2019, approximately 1.9 million Americans aged 12 or older had cocaine use disorder in the past year (44).
Methamphetamine Use Disorder:
A study published in Drug and Alcohol Dependence reported that the prevalence of methamphetamine use disorder in the United States was estimated to be 0.2% in 2015-2016 (6).

Self Quiz
Ask yourself...
- What are the options available for managing opioid addiction and withdrawal?
- How can nurse practitioners support patients in their recovery from opioid addiction?
- What strategies can nurse practitioners employ to effectively engage and build trust with patients reluctant to disclose or seek help for substance abuse disorders?
- How can nurse practitioners collaborate with other healthcare professionals and community resources to provide comprehensive care and support for patients with substance abuse disorders?
- What techniques or tools can nurse practitioners employ to start these sensitive conversations with new patients?
- How do you assess and manage patients experiencing opioid withdrawal symptoms?
- What are the non-pharmacological interventions for managing opioid withdrawal?
- How do you educate patients about the risks and benefits of addiction medications?
- How do you monitor patients on addiction medications for adherence and progress?
- What are the drug potential interactions with commonly prescribed addiction medications?
Drug Diversion and Illegal opioids
Misuse of opioids is facilitated by diversion and is defined as "the transfer of drugs from lawful to unlawful use" (24). Most commonly, this occurs when family and friends share prescribed opioids with other family and friends. Opioids and other controlled drugs are also diverted from healthcare facilities. Statistics show that healthcare facility diversion has increased since 2015 (24)
Diversion affects patients, healthcare workers, healthcare facilities, and public health. Patients experience substandard care due to ineffective pain management and impaired healthcare workers. In addition, affected patients are at risk of infections from compromised syringes (24).
Healthcare employees who divert are at risk of overdose and death. If caught, they face criminal prosecution and malpractice suits. Healthcare facilities also bear the cost of diverted drugs via internal investigations, follow-up care for affected patients, regulatory fines for inadequate safeguards, and declining public trust (24).
Despite the enormous consequences of drug diversion, healthcare facilities have implemented few processes to detect and deter the diversion of controlled substances (24).

Self Quiz
Ask yourself...
- What protocols can nurse practitioners implement to prevent drug diversion within their healthcare setting?
Patient Teachings and Considerations
Opioids have significant side effects and carry a risk of addiction and overdose. Nurse practitioners can decrease the risks of misuse and addiction by educating patients on appropriate disposal, safe storage, and potential signs of addiction. Taking additional time to provide teaching nurse practitioners can promote patient safety, informed decision-making, and responsible opioid use.
Safe Storage and Disposal:
- Teach patients to store opioids securely, out of reach of children, pets, visitors, and non-caregiver family members, to prevent accidental ingestion or misuse (13). Only the caregiver, if applicable, or the patient should have access to pain medications.
- Instruct patients on proper disposal methods, such as using drug take-back programs or mixing opioids with undesirable substances (e.g., coffee grounds) before throwing them away (11) (13).
Medication Adherence:
- Emphasize the importance of taking opioids as prescribed, at the correct dose and frequency, to achieve optimal pain relief.
- Encourage patients to notify their healthcare provider if they experience inadequate pain control or side effects (35).
Potential Side Effects:
- Educate patients about common side effects of opioids, including constipation, nausea, sedation, and respiratory depression.
- Discuss strategies to manage side effects, such as maintaining adequate hydration, consuming a fiber-rich diet, and using over-the-counter laxatives as needed (11).
Risk of Dependence and Addiction:
- Explain the potential for opioid dependence and addiction, especially with long-term use or a history of substance abuse.
- Encourage patients to promptly report signs of opioid misuse, such as craving, loss of control, or continued use despite negative consequences (51).

Avoiding Alcohol and Other Central Nervous System Depressants:
- Instruct patients to avoid consuming alcohol or other medications that can enhance the sedative effects of opioids, increasing the risk of respiratory depression.
- Advise patients to contact the Nurse Practitioner before starting new medications, including over-the-counter drugs or herbal supplements (2).
Driving and Operating Machinery:
- Inform patients about the potential impairment caused by opioids, including reduced alertness, reaction time, and coordination.
- Advise patients to avoid driving or operating heavy machinery while taking opioids until they know how the medication affects them (14).

Self Quiz
Ask yourself...
- What strategies can nurse practitioners employ to effectively communicate the risks and benefits of opioid use while ensuring they clearly understand the potential side effects and the importance of adhering to the prescribed regimen?
- How can nurse practitioners promote patient engagement and shared decision-making regarding opioid pain management, considering the potential for dependence and addiction?
- How can nurse practitioners assess a patient's knowledge and understand the safe storage and disposal of opioids?
Case Study
You take some extra time with Mary to educate her on the taper dose of Vicodin, the potential for harm, and the risk of opioids, especially when used concomitantly with Gabapentin. You let Mary know it is unsafe to use alcohol, not only with Vicodin but also with Gabapentin. You let Mary know that Vicodin has a risk of dependency and misuse and, therefore, she will be monitored carefully. You also educate that Mary should store the Vicodin away from visibility by anyone but herself since she can self-administer her medication. You let Mary know that Vicodin can cause constipation and that she should increase her water intake and take a stool softener.
You ask Mary to call you if her pain is not adequately relieved or if her medications run out before the three days.
You let Mary know that if she does stop taking the Vicodin before she has completed all the medication, she should dispose of it by mixing the pills with liquid and coffee grounds to make them unpalatable to animals and others.
Mary complied with your education, completed her course of Vicodin, and was scheduled for surgery. Mary's social worker helped her communicate with her new employer and delayed her start date until after her recovery.
During her recovery, Mary received physical therapy and a short course of pain medication managed by her orthopedist.
Mary returned to the clinic for a follow-up visit after completing her therapy and before starting work. Mary's pain level in her knee is 3/10, and she already feels like she can walk further than pre-surgery. Gabapentin has continued to help Mary's neuropathic pain in her back, and she reports 2/10. Mary looks forward to beginning her new job and is optimistic about the future.
Conclusion
Pain management is the leading cause of primary care appointments and chronic pain is the leading cause of disability. Yet, prescribing opioids for primary care patients is also a factor in drug misuse and the opioid epidemic. Nurse practitioners are challenged to appropriately treat pain and effectively control diversion, addiction, and death from overdose.
It is imperative that nurse practitioners use evidence-based practices to assess, appropriately intervene, and educate about the benefits and potential harm caused by treatment with opioids. Nurse practitioners must stay up to date with the current federal regulations regarding PDMPs, clinical prescribing guidelines, and emerging treatments for pain and opioid abuse disorders.
Tirzepatide for Type 2 Diabetes and Weight Management
Introduction
The emergence of the drug tirzepatide is becoming more popular and widespread and is being utilized among those with diabetes and also those who desire to lose weight. It is one of the newest diabetic drugs given by injection that also triggers dramatic weight loss in those who use the injections.
The U.S. Food and Drug Administration (FDA) approved tirzepatide in 2022 for individuals with diabetes, particularly Type 2 Diabetes. The FDA officials have not approved tirzepatide yet for weight loss, but they are currently tracking the medication and may have a recommendation for its approval by the end of this year. Clinical trials have shown that individuals with an elevated body mass index (BMI) and who did not have diabetes lost a considerable amount of weight when they received tirzepatide (1).
Advanced Practice Registered Nurses (APRNs) need to understand how to safely prescribe tirzepatide and the reasoning as to why it causes weight loss for specific individuals.
Drug Classification
Tirzepatide is part of a class of medications called glucose-dependent insulin tropic polypeptide (GIP) receptor and glucagon-like peptide-1 (GLP-1) receptor agonists. It comprises a 39 amino acid linear synthetic peptide conjugate to selective receptor agonists in preclinical and clinical trials.
Tirzepatide is used for treating Type II diabetes in adults as an adjunct to diet and exercise. It is also used for weight loss in some individuals and has gained increased attention as a new therapeutic agent for glycemic and weight control.
Social media has had a significant influence and increased the desire to use tirzepatide, and while individual results vary, the weight loss in adults ranged from 12 – 25 pounds.
Online pharmacies, diet clinics, and medical spas are implementing thousands of ads on social media to capitalize on a surge of interest in the drug.

Self Quiz
Ask yourself...
- Why has there seemed to be an increase in patients requesting this medication? What other medicines intended for type 2 diabetes are also being used for weight loss management?
- What are the ethical considerations regarding marketing this drug for weight loss when its primary use is for type 2 diabetes? Could this impact supply and costs?
Indications of Usage
The use of tirzepatide is being used for both Type II diabetes and weight control in certain patients. It has been a game changer for people living with Type II diabetes. The drug’s primary use is as an adjunct to diet and exercise to improve glycemic control in adults with diabetes.
The drug has also proven beneficial for weight loss in patients experiencing obesity, and those who are taking the highest dosage have shared a body weight reduction of 15.7% (2). Tirzepatide is an injectable prescription medication used together with diet and exercise, and it is not yet known if it can be used safely with patients who have had pancreatitis.
It is important to remember that it is not to be used for patients with Type I diabetes, but it is safe for Type II diabetic patients. Also, the safety of tirzepatide has yet to be discovered for children and those under 18; therefore, the medication should not be used for this age group.
In studies conducted with or without diabetic medicines, 75% – 90% of patients taking tirzepatide reached an overall A1C of less than 7% with an average starting A1C of 7.9 – 8.6% across the following dosages – 5mg, 10mg, and 15mg. The study results were measured at weeks 40 and 52 (3).

Self Quiz
Ask yourself...
- What dietary and activity recommendations can you provide to patients using tirzepatide for weight loss?
- Is this drug intended for those who want to lose 5-10 pounds?
Use of Tirzepatide with Diabetic Patients
Tirzepatide can be used for patients with Type II diabetes in combination with a diabetic-friendly diet and exercise. The drug works by lowering the patient’s overall blood sugar and also improves the A1C results of patients over some time. The injection has been approved by the FDA to treat Type II diabetes and is administered once weekly (4).
It is considered the first in a new class of medications – a dual glucose-dependent insulin tropic polypeptide (GIP) and glucagon-like-peptide-1 (GLP-1) receptor antagonist. The mechanism of how it works mimics two gut hormones (GIP and GLP-1). These hormones are essential in how patients digest food and regulate blood glucose after meals. The hormones also play a role in making individuals feel fuller and curb specific food cravings.
The provider can prescribe tirzepatide before attempting other diabetic medications if a patient has a BMI of 30 or greater or 27 or greater with weight-related conditions and if the drug is combined with a personalized weight loss plan that addresses physical activity, nutrition, and lifestyle changes.
However, due to the cost and some insurance companies not covering the injection unless the patient has both diabetes and obesity, the provider must carefully consider prescribing this medication.

Case Study
The patient states this ‘miracle drug’ is worth paying for out of pocket!
Jeff Capron, a 53-year-old Boonville, New York, web developer, started taking tirzepatide in December 2022. His friend had reported good results with the medication, so Jeff looked into the research studies behind it and then spoke with his primary physician.
The physician said, “Yeah, let’s give it a shot,” even though he did not have much experience with it. The physician did not have an opinion one way or the other than looking at the data set and seeing no reason why they could not try it.
Jeff’s hemoglobin A1C went from 10.1% to 6% in 3 months, which was very promising. “I never had that kind of experience with any medication for diabetes.” There is a range in how much A1C reduction people experience with tirzepatide, but many people taking it can get their A1C under 7% — an ideal goal for people with Type 2 diabetes.
Jeff experienced constipation and a little trouble sleeping early, but both issues disappeared quickly. He says, “I wake up in the morning, and my fasting blood sugars are normal.”
The medication took effect, he says, within 12 hours. He compared the feeling to having a gastric bypass.
“You cannot overeat food. As soon as you overeat, you almost feel ill.” While it generally takes a few months to notice effects like A1C reduction and significant weight loss, side effects such as lower appetite may be felt immediately.
Weight loss was not his primary goal, but he lost about 35 pounds on the medication in the first five months. He also lost his sweet tooth. “I can maybe count three sweet things I have eaten since December.”
Jeff found that his appetite slowly recovered days after taking tirzepatide. “You take the shot every Sunday, and by Saturday, you start to get a lot of appetite,” he says. “It does not seem to affect your weight. If I eat a little bit more on Saturday night, on Sunday, the scale will not move one way or the other.”
Jeff is allergic to hornets, so he already carries an auto-injector. He was not worried about using another drug delivered through a needle. “It’s just a push button,” he says. It also helped that his wife is a nurse. “So, I had her with me the first time to ensure I was doing it right. I didn’t even feel it.”
When Jeff was first prescribed tirzepatide, his insurance covered it. The company has since removed that benefit. He has filed an appeal but pays about $1,000 monthly out of pocket for his weekly injections. He plans to keep paying as long as necessary.
He considers the financial burden well worth it. “I have never had a medication that worked as well before for chronic conditions,” Jeff says. “I’ve been blown away by it. For me, it’s a miracle drug. It got rid of my diabetes” (4).

Self Quiz
Ask yourself…
- Can a provider willfully choose to prescribe tirzepatide before other diabetic medications are attempted?
- Would that impact his insurance coverage if Jeff did not meet the clinical criteria for using tirzepatide?
Use of Tirzepatide for Weight Loss Management
As mentioned, this medication is indicated for patients with a BMI of >30 or a BMI of >27 with qualifying comorbidities. Obesity can become a chronic lifetime disease, and for conditions such as these, the patient needs to implement therapy for the lifetime of the disease.
In a study conducted for tirzepatide, there was a dramatic increase in effectiveness compared to traditional nonsurgical interventions such as diet, exercise, and lifestyle changes. However, it has been noted that taking tirzepatide on an ongoing basis is recommended and necessary to maintain any weight loss achieved from the medication.
If a patient stops taking the drug, likely, it will no longer work (5).
Public health officials have expressed concerns about using the drug long-term. Still, data is currently lacking regarding long-term effectiveness, treatment duration, and maintaining weight reduction once the therapy is discontinued.
A recent trial consisted of 783 participants with a BMI greater than 30, and these participants agreed to take either a 10mg or 15mg dose of tirzepatide over 36 weeks. The injection is given once weekly, so this would equal a total of 36 injections.
By the end of 36 weeks, participants lost more than 21% of their body weight. After 36 weeks, participants continued on tirzepatide or received placebo treatment for the following year. The patients needed to be made aware of which treatment they were receiving.
Those still taking tirzepatide injections weekly after 88 weeks lost an additional 7% of their body weight, and those taking the placebo regained 15% at the end of 88 weeks (5).

Self Quiz
Ask yourself…
- What is the minimum BMI needed to qualify to receive this drug for weight loss management?
- Is this medication indicated for long-term use for patients with a high BMI?
Common Side Effects and Contraindications
Side Effects
Patients vary immensely with different experiences and side effects related to tirzepatide; however, the following are the most common side effects experienced by those taking the medication:
- Nausea
- Decreased appetite
- Vomiting
- Diarrhea
- Indigestion
- Constipation
- Stomach Pain
Tirzepatide usually does not cause fatigue, leaving one feeling weak, tired, and low energy. However, fatigue can be a common side effect of Type II diabetes.
It is important to note that most individuals who experience nausea, vomiting, and diarrhea episodes do so while the dosage increases, and typically, the symptoms decrease over time. G.I. effects were more prominent in those taking tirzepatide than those taking the placebo. The individuals not in the placebo group were more likely to stop treatment due to the unpleasant side effects (3).


Self Quiz
Ask yourself...
- Does tirzepatide cause fatigue in patients who use it?
Contraindications
Tirzepatide may cause thyroid tumors, including thyroid cancer, and it is essential to watch for possible symptoms, such as swelling or a lump in the neck, hoarseness, shortness of breath, or trouble swallowing.
Tirzepatide should also not be prescribed to any patient with Type 1 Diabetes.
One of the main ways that tirzepatide works is by stimulating the release of insulin from the pancreas, and due to this fact, there have not been many studies and clinical trials that include those with Type I diabetes.
However, this is not to say that prescribers have never ordered tirzepatide for those with Type I diabetes. Still, it is essential to note that if prescribed, it would be in addition to traditional insulin therapy.
- Personal or family history of a type of thyroid cancer known as medullary thyroid carcinoma (MTC).
- Any history of Multiple Endocrine Neoplasia syndrome type 2 (MEN 2).
- Patients who are allergic to the actual medication or any of its ingredients.
- Younger than 18 years of age


Self Quiz
Ask yourself...
- What is the reason that tripeptide is contraindicated in those with Type I diabetes?
- Why is there a risk with patients who have a thyroid disorder?
Safe Prescribing Practices, Guidelines, and Considerations for Providers
Safe Prescribing Practices
As with all prescribed medications, safe standards of care must be implemented and followed to ensure patient safety is maintained. The same applies to providers considering prescribing tirzepatide, and specific criteria must be met beforehand. The following information discusses guidelines involving exclusion and inclusion criteria for providers to prescribe tirzepatide (6) accurately.
Guidelines
Exclusion Criteria – If present, the following indicates that the patient should not receive tirzepatide:
- Diagnosis of Type I diabetes
- Personal or family history of medullary thyroid carcinoma or with Multiple Endocrine Neoplasia syndrome type 2
- Severe gastrointestinal dysmotility
- History of pancreatitis
- Pregnancy
- Proliferative Diabetic Retinopathy (PDR), severe Nonproliferative Diabetic Retinopathy (NDR), clinically significant myalgic encephalomyelitis (M.E.), or diabetic macular edema (DME) unless the risks/benefits have been discussed with the patient and are documented in the patient's health record along with monitoring plans and follow-up with an eye specialist who is informed at the time of initiation.
Inclusion Criteria – All of the following must be met for tirzepatide to be prescribed:
- Diagnosis of Type II diabetes
- A BMI of 25 or greater
- Inadequate glycemic control on at least 1mg of semaglutide injection plus two or more glucose-lowering drugs
- Change needed to achieve goal A1C is less than 1%.
- Goal A1C should be based on those recommended in the Diabetic Guidelines.
- Adherence to current diabetic medications as evidenced by a review of the prescription refill history during the six months.
Additional Inclusion Criteria – All of the following must be met for tirzepatide to be prescribed:
- Patients with atherosclerotic cardiovascular disease or chronic kidney disease
- Patients of childbearing potential who are using oral contraceptives
Inclusion Criteria for Weight Loss
- BMI of >30 or >27 with patient weight conditions.

Self Quiz
Ask yourself...
- Would a patient with a BMI of 23 with no comorbidities qualify to use tirzepatide to lose 5-10% of their body weight? Why not?
- What impact can tirzepatide have on a person with a healthy weight and BMI of <25?
Considerations for Providers
There are specific considerations that prescribers must be aware of when contemplating if a patient should receive the medication tirzepatide. The following is imperative and must be considered each time the medication is prescribed to a patient:
- Clinical Indications – indicated for treating adults with insufficiently controlled diabetes mellitus as an add-on therapy to diet and exercise; as monotherapy when metformin is considered inappropriate due to contraindications or intolerance; and other medicinal products for treating Type II diabetes.
- Monitoring of medication – routine monitoring of serum calcitonin or thyroid ultrasound is of uncertain value but is recommended for early detection of Medullary Thyroid Cancer (MTC).
- Cost – the average price for tirzepatide ranges from $1,071-$1,351 without any coupons or insurance. Savings Card – manufacturer provided; patients can pay as little as $25 monthly for up to 12 injections. Savings Card – manufacturer provided; patients can pay as little as $25 monthly for up to 12 injections.
- Benefits and Risks – One must evaluate the effectiveness of diabetes and the weight loss experienced. Some of the risks must be evaluated, such as increased cost of medication, unpleasant gastrointestinal side effects, poor insurance coverage, and drug shortages. The FDA has warned that the medicine can cause thyroid C-cell tumors in rats, and it is not sure whether tirzepatide causes similar tumors.
How long does it take for tirzepatide to begin working?
Tirzepatide will start to lower one's blood sugar levels immediately, but it can take 8 to 12 weeks to reach one's target A1C goal.
Compared to other diabetic treatments, studies have shown that it can take eight weeks to reach an A1C target of less than or equal to 7% and 12 weeks to get an A1C of less than or equal to 6.5%. Significant weight loss can occur as early as 28 weeks.
Safe Administration
It is essential to follow the correct steps for safe administration of tirzepatide as listed below:
- The recommended starting dosage is 2.5mg, injected subcutaneously once weekly. The 2.5mg dosage is for treatment initiation and not for glycemic control.
- After four weeks, increase the dosage to 5mg, injected subcutaneously once weekly.
- If additional glycemic control is needed, increase the dosage in 2.5mg increments after at least four weeks on the current dose.
- The maximum dosage is 15mg, injected subcutaneously once weekly.
- If a dose is missed, instruct patients to administer it as soon as possible, within four days (96 hours) after the missed dose. If more than four days have passed, skip the missed dose, and administer the next dose on the regularly scheduled day. In each case, patients can then resume their regular once-weekly dosing schedule.
- The day of weekly Administration can be changed, if necessary, as long as the time between the two doses is at least three days (72 hours).
- Before initiation, train patients and caregivers on proper injection techniques.
- Instruct patients using the single-dose vial to use a syringe appropriate for dose administration (e.g., a 1ml syringe capable of measuring a 0.5 mL dose).
- Administer the medication once weekly, any time of day.
- Inject the medication subcutaneously in the abdomen, thigh, or upper arm.
- Rotate injection sites with each dose.
- Inspect the medication visually before use. It should appear clear and colorless to slightly yellow. Do not use the medicine if particulate matter or discoloration is seen.
- When using the medication with insulin, administer it as separate injections and never mix. It is acceptable to inject tirzepatide and insulin in the same body region, but the injections should not be adjacent.
Does the tirzepatide injection hurt when administered?
Pain from the injection site has not been reported as a common side effect, but it may occur.
Due to the injection being given subcutaneously, slight pain or discomfort can occur.


Self Quiz
Ask yourself...
- The patient asks you," How long will this take to work?" How will you respond?
- The patient reports they have never used an injection before; what methods can you use to teach your patient how to administer this medication safely?
Alternatives to Tirzepatide for Weight Loss Management
In some instances, patients need to be aware of alternatives to tirzepatide in case they cannot take the actual injection for whatever reason. In cases such as these, there are alternative supplements that can be purchased over the counter, and they include the following (7):
- PhenQ – top OTC choice – comprehensive weight loss solution that targets specific body regions, facilitates prompt fat loss, and expedites the weight loss journey.
- PhenGold – the most potent OTC weight loss alternative – one of the top weight loss supplements that boost metabolism, making one less hungry, less tired, and an overall improved feeling.
- Capsiplex BURN – the best choice for men – helps to burn fat faster and keep blood sugar levels in check. It helps to keep one's muscles, curbs hunger, gives one more energy, and torches stubborn fats.
- Trimtone – the best choice for women – helps women to lose weight, eat less, increase metabolism, burn extra calories, and boost energy.
- Prime Shred – best fat burner for men – boosts metabolism, keeps muscles intact, increases energy, and helps maintain focus.
The advanced practicing nurse or prescriber needs to inform patients about alternative options such as these in an effort for individuals to understand that other choices are available and can be used. Many individuals need to be more knowledgeable about alternatives besides tirzepatide due to the extra hype from social media sources that promote advertisements related to tirzepatide only but do not mention the other options.
Why does social media influence and encourage patients to take tirzepatide?
Social media trends can be helpful but can also become harmful by setting unrealistic expectations and promoting a diet culture mentality. They can create an unhealthy obsession with "clean" eating, especially in the younger populations.
Due to this, many individuals take the medication despite any occurrence or history of Type II diabetes, and the drug can ultimately become misused.
It has been noted that there is an influx of patients requesting this medication for weight loss instead of the intended purpose, which is to help control Type II diabetes.
Tirzepatide represents one of the most recent non-medical treatments aimed at managing the symptoms of Type II diabetes. While it is not indicated for weight management, diabetic patients who receive it frequently report a significant reduction in body weight.
Empirical evidence suggests the efficacy of tirzepatide in weight management, and certain physicians currently endorse the Administration of the medication as a therapeutic and effective means to overcome obesity.
What are some severe side effects of tirzepatide that can impact patient safety?
The Administration of tirzepatide can benefit many individuals, but some severe side effects must be mentioned.
These include thyroid tumors, thyroid cancer, pancreatitis, hypoglycemia, serious allergic reactions, kidney issues, severe stomach problems, vision changes, and gallbladder issues. All these side effects must be taken seriously and reported, as they can lead to life-threatening

Self Quiz
Ask yourself...
- With what you have learned in this course, what education will you provide to patients requesting this medication for weight loss?
- Have you seen increased demand for this medication in your current practice?
- If you Google tirzepatide, your results will likely include links to telehealth services promoting this weight-loss medication. To determine eligibility, what special considerations need to be taken to assess a telehealth patient?
Conclusion
Medications like tirzepatide are game changers for those patients with type 2 diabetes that have failed other medications. Unfortunately, several companies seek to profit from its weight-loss benefits through aggressive marketing campaigns that limit the available supply and increase the costs for those who need it. As healthcare providers, we need to use sound clinical judgment and follow the exclusion/inclusion criteria and other guidelines before prescribing this medication, so we do not unintentionally cause harm while looking to appease our patients who request this.
Semaglutide and Type 2 Diabetes
Introduction
In 2017, the FDA approved the semaglutide injectable (Ozempic) for treating type 2 diabetes. The drug has experienced widespread acceptance due to its positive effects on weight loss and lowering of chronic health risks. The drug has risen in popularity over the past few years, as many well-known actors/actresses/songwriters, and more came forward, publicly sharing their weight loss journey.
This rise in popularity has also resulted in significant shortages of this medication, negatively impacting the lives of the diabetic community, local pharmacies, and healthcare providers. The goal of this continuing education course is to educate and empower the healthcare provider in all aspects of this drug regimen: clinical indications, patient education, cost options, and benefit/risk analysis.
Diabetes Overview
Diabetes is a chronic medical condition. Despite advances in diet, medications, and monitoring devices, diabetes diagnoses continue to grow at staggering rates. The Institute for Health Metrics and Evaluation (IHME) reports that over 529 million people worldwide are currently living with diabetes, and that number is expected to grow to 1.3 billion in only 30 years. While the risk factors for diabetes are vast in number (poor diet, inadequate activity, obesity, sedentary lifestyles, daily stressors, and more), the sad reality is that this chronic medical condition will most likely linger on for generations to come despite our efforts to contain this health epidemic (1).
According to the latest research on diabetes, there are over 37 million people in the United States alone with diabetes as of 2022. Statistically, approximately 28 million of them have a confirmed diagnosis, while another estimated 8 million are experiencing symptoms, without an official diagnosis. Diabetes currently ranks as the 7th leading cause of death in the United States (2).

Self Quiz
Ask yourself...
- As a healthcare provider, what has been your experience with treating chronic medical conditions?
- Why do you think there is a continued increase in diabetes, despite advances in medication and monitoring devices to treat this condition?
- Are you currently offering comprehensive care to your patients, including medication, diet, and activity counseling for their chronic health conditions?
Types of Diabetes
In basic terms, diabetes is an impairment in one’s ability to either adequately produce or utilize insulin, which results in elevated levels of circulating glucose. Chronically elevated glucose levels affect blood vessels at every level, causing chronic inflammation and raising the risk of heart disease, stroke, blindness, and atraumatic amputations.
There are three main types of diabetes:
Type 1 diabetes is thought to be an autoimmune disease. Approximately 5-10 percent of people with diabetes are diagnosed with type 1 diabetes. The diagnosis usually occurs in early childhood, and results in a lifetime use of insulin to regulate blood glucose levels.
Type 2 diabetes is thought to be related to dietary and lifestyle choices. It accounts for nearly 90-95 percent of diabetes diagnoses. Usually occurring later in life (adult-elderly population), it is believed to be related to factors such as diet, activity, weight gain, and related factors. Type 2 diabetes is usually controlled by diet and exercise, in addition to oral medications, although injectable insulin may be included in the treatment plan.
Gestational diabetes refers to elevated glucose levels occurring during pregnancy for patients who are not diabetic at the onset of pregnancy. This version of diabetes usually resolves itself post-partum, although a woman may develop type 2 diabetes later in life, unrelated to pregnancy.
Type 2 diabetes in children: no longer a “later in life diagnosis”
Children are now being diagnosed with type 2 diabetes at an alarming rate. Despite widespread education and an increased awareness of diabetes, our up-and-coming generation is unhealthier than ever. Many families lack access to healthy food for their families, due to both general socioeconomic challenges and an increased rate of food insecurity. (19)
The CDC recommends care providers have resources for diabetic patients and their families, such as food and nutrition programs, budget-friendly diabetes meal plans, how to save money on diabetes care, and coping strategies for diabetes. (19)


Self Quiz
Ask yourself...
- Are you able to articulate the different types of diabetes to patients?
- What resources can you offer to the families of children with type 2 diabetes?
Diabetes Signs and Symptoms, Diagnostic Testing
There are various ways to test for diabetes. The fasting blood sugar (FBS)/ fasting glucose level is a simple way to test for diabetes.
The normal fasting glucose level is below 100mg/dl. The fasting glucose result of 100-125mg/dl indicates prediabetes and results above 126mg/dl indicate diabetes.
The hemoglobin A1C blood test is another test used to confirm the diagnosis of diabetes. The patient does not need to be fasting for this test; thus, it is easier to order this test regardless of the time of day. This blood test reflects the average glucose level over the period of 2-3 months.
The normal A1C level is below 5.7%. Test results between 5.7%- 6.4% indicate prediabetes. Test results above 6.5% indicate diabetes.
A random glucose reading above 200mg/dl, done at any time of day, indicates diabetes.
The diagnosis of diabetes is by blood tests, and for improved accuracy, should be based on two separate readings, done (at least) a day apart. In the case of fasting and random blood tests, dietary intake (large amounts of carbohydrates in a single meal) may adversely affect test results. This is not the case when using A1C testing for a confirmation diagnosis, as the results are the average of a 2–3-month span.
Target blood levels for a person with diabetes (3).
Target blood glucose levels for people with diabetes are as follows:
- Fasting glucose 80-130mg/dl.
- Postprandial blood glucose level- less than 180mg/dl
- A1C level 7-8%.
These target ranges are general guidelines. Patient-specific ranges will be dependent on a variety of factors, including preexisting comorbidities, overall health status, age, and activity levels.

The hallmark signs/symptoms of diabetes
- Polyuria- increased urination
- Polydipsia- increased thirst
- Polyphagia-increased hunger/appetite
The truth is, as healthcare providers, you will have patients who have no hallmark signs and symptoms of diabetes; the diagnosis will be found during annual preventive examinations often unrelated to any chronic disease. For this reason, many insurance companies now cover numerous preventive screenings, including diabetes screenings, as part of their wellness and prevention initiatives. These tests are often approved based on a patient's age, or preexisting conditions, rather than outright signs and symptoms.

Self Quiz
Ask yourself...
- What are the typical glucose levels for non-diabetic versus diabetic patients?
- What are the hallmark symptoms you can identify when treating a potentially diabetic patient?
Lifestyle Interventions and the Diabetes Prevention Program
The initial diagnosis of diabetes can be managed in a variety of ways, depending on the severity of the illness at the time of diagnosis. Lifestyle interventions (behavior modification education) are of utmost importance in the care and management of people with diabetes. Research over the past few decades has consistently shown that such interventions have immense positive effects on the successful long-term management of diabetes.
The official Diabetes Prevention Program was created in 2010 (4) and confirmed the effects of lifestyle interventions in the management of diabetes: Lifestyle interventions decreased the incidence of type 2 diabetes by 58% compared with 31% in the metformin-treated group. Thus, these findings now serve as the blueprint, if you will, for all-inclusive, patient-specific disease management guidelines. These lifestyle interventions will be discussed in detail later in the program.
Additional Resources on Diabetes Prevention

Self Quiz
Ask yourself...
- How do lifestyle interventions compare to other kinds of treatment for patients with type 2 diabetes?
Semaglutide
Semaglutide is an injectable drug used in the treatment of type 2 diabetes. It was approved by the FDA in May of 2017.
It is a once-a-week injectable and belongs to the drug class known as glucagon-like peptide-1 receptor agonists (GLP-1RAs) (5). It has been referred to as a “miracle weight loss drug” among those who are living with obesity, despite frequent side effects, unusually high out-of-pocket costs, drug shortages, and weight regain when attempting to stop using the medication.
GLP-1 receptor agonist: Hormone Review
GLP-1 RAs are a class of medications used to treat Type 2 diabetes, and in some cases, obesity treatment. They are also known as GLP-1 receptor agonists, incretin mimetics, and GLP-1 analogs.
Ghrelin and Leptin (6)
Ghrelin and Leptin are two hormones that greatly influence appetite and the sensation of fullness. Often referred to as the “hunger hormone.” Ghrelin is responsible for many functions, including playing a key role in metabolism through glucose and insulin regulation.
Ghrelin, produced in your stomach, signals your brain when you are hungry, and results in increased food intake.
Leptin, conversely, is produced in your fat cells, and signals to the brain when you have eaten enough (by a decrease in appetite).
Glucagon-like peptide-1 receptors
Known as GLP1 receptors, Glucagon-like peptide-1 receptor proteins are located in the beta cells of the pancreas as well as in the neurons in the brain. GLP-1 receptors are involved in the regulation of blood glucose levels and affect the secretion of insulin. These cells encourage the release of insulin from the pancreas, increase the volume of beta cells, and reduce the release of glucagon. In doing so, they increase the feeling of fullness during and between meals, suppressing the appetite and slowing gastric emptying.

Self Quiz
Ask yourself...
- What are some problems patients might face if they choose to take semaglutide?
- How do Ghrelin and Leptin relate to a patient's appetite?
What is meant by receptor agonist and antagonist?
The term agonist refers to any substance that mimics the actions of a hormone in producing a specific response: a receptor antagonist blocks a response from occurring.
Opioids are examples of receptor agonists in that they produce responses such as analgesia.
Naloxone/Narcan is an example of a receptor antagonist, in that it binds to a receptor site and decreases/blocks a response from occurring.
Semaglutide mechanism of action (7)
GLP-1 agonists work in several ways to positively affect glucose levels. Their mechanism of action includes the following:
- Increasing (stimulating) insulin secretion by the pancreatic beta cells.
- Decreasing the production of glucagon, a hormone that raises blood glucose levels
- Decreasing (slowing) gastric emptying
- Decreasing appetite (and thereby reducing food intake) by creating a sensation of stomach fullness
Through these mechanisms of action, semaglutide results in a lowering of serum glucose/A1C levels, which lowers the risk of cardiovascular events. Studies have also shown that semaglutide resulted in weight loss (approximately 8-14 pounds on average {dose dependent results}.

Self Quiz
Ask yourself...
- What is the difference between an agonist and antagonist substance?
- How much weight do patients lose, on average, when taking semaglutide?
Side Effects of Semaglutide
Common side effects of semaglutide (8)
Common side effects may include any of the following:
- Nausea and vomiting
- Headache
- Diarrhea and stomach pain
- Upset stomach, indigestion, constipation, flatulence
These side effects usually subside within a few weeks, as the patient becomes acclimated to the medication.
Serious side effects of semaglutide
- Hypoglycemia- enhanced/worsened when used in combination with other diabetes medication. Symptoms may include drowsiness, confusion, weakness, irritability, and headache.
- Symptoms may include abdominal pain and distension, nausea and vomiting, fever, and back pain.
- Diabetic retinopathy. Symptoms may include blurred vision, vision loss, and diminished night vision.
- Kidney damage/injury/failure. Symptoms may include fatigue, nausea, diminished urine output, confusion, and edema of extremities.
- Gallbladder disease. Symptoms may include gallstones, abdominal pain, nausea and vomiting, and poor appetite.
Black Box Warning (9)
Semaglutide has a Black Box Warning for thyroid cancer. This is the most serious warning from the Food and Drug Administration (FDA) and is intended to alert consumers to the potential risks of a medication. This black box warning was issued when research found that the drug increased the risk of thyroid tumors in animals.
It is not known if semaglutide actually causes tumors in humans.
Contraindications
- Semaglutide is contraindicated in people with a personal or family history of MTC (medullary thyroid cancer) or in patients with multiple endocrine neoplasia syndrome type 2.
- Known hypersensitivity to semaglutide or any of the product components
Cautions
As noted under “serious side effects”, there have been reports of new illnesses or worsening of existing health conditions occurring “post-marketing”. Thus, healthcare providers are strongly encouraged to continue ongoing surveillance of any patients on semaglutide therapy. In addition, there is insufficient data available regarding the use of semaglutide by pregnant women. Women are therefore highly encouraged to stop any treatment with semaglutide for at least 2 months prior to a planned pregnancy.

Self Quiz
Ask yourself...
- Can you name the 4 common side effects of semaglutide?
- What is the most severe warning associated with semaglutide?
Dosing
Semaglutide is indicated as an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus (T2DM). It is looked upon favorably to reduce the risk of cardiovascular events in adults with T2DM and a preexisting history of cardiovascular disease. This drug is FDA-approved for use in people with diabetes, with a BMI of 27% or higher (a BMI of 25-29.9% is considered overweight).
Semaglutide (Ozempic) is available as an injectable prescription medication. Doses include 0.5mg, 1mg, or 2 mg, once weekly.
The injection should be administered subcutaneously to the abdomen, thigh, or upper arm. Injection sites should be rotated, and given as a single injection.
Start at 0.25 mg once weekly. After 4 weeks, increase the dose to 0.5 mg once weekly.
- If additional glycemic control is needed, increase the dose to 1 mg once weekly after at least 4 weeks on the 0.5 mg dose.
- If additional glycemic control is needed, increase the dose to 2 mg once weekly after at least 4 weeks on the 1 mg dose
Administer once weekly at any time of day, with or without meals. The maximum dose recommendation is 2mg/weekly once weekly.
Note: The initial 0.25-mg dose is intended for treatment initiation and is not effective for glycemic control
Missing Dose Guidelines
- If the missed dose is ≤5 days: Administer dose as soon as possible
- If missed dose >5 days: Skip the missed dose and administer the next dose on the regularly scheduled day; patients can then resume their regular once-weekly dosing schedule
Administration Day Guidelines (10).
The administration day each week can be changed, if necessary, as long as the time between 2 doses is at least 2 days (>48 hours)
Dose Availability (packaging)
- 2mg/1.5mL (1.34mg/mL); delivers doses of 0.25mg or 0.5mg per injection or four to eight doses per injection pen
- 4mg/3mL (1.34mg/mL); delivers 1mg per injection or 4 doses per injection pen
- 8mg/3mL (2.68 mg/mL); delivers 2mg per injection or 4 doses per injection pen
Treatment Goals- Effects on A1C and Weight (11)
A majority of adults who were placed on injectable semaglutide for diabetes management achieved a target A1C under 7% and were able to maintain it.
- Dose specific effects on A1C were as follows:
- 0.5mg dose injection yielded a 1.4% decrease
- 1.0mg dose injection yielded a 1.6% decrease
- 2.0 mg dose injection, in combination with diabetes pills, yielded a 2.1% decrease in A1C.
Adults taking semifluid injectables for diabetes management also noted weight loss.
- 8-pound weight loss reported with 0.5mg dose injection
- 10 pounds weight loss reported with 1.0mg dose injection
- Up to 14 pounds of weight loss reported with a 2.0mg dose injection


Self Quiz
Ask yourself...
- What should you tell a patient if they miss their injection by more than 5 days? What if it has been less than five days?
Prescribing insights: Long-Term therapy for a chronic condition?
Semaglutide is viewed favorably as a treatment option for Type 2 diabetes. It appears to lower A1C levels and body weight in the majority of patients, lowering their risk of future cardiovascular events.
The question of long-term medication use, for a chronic health condition, is being heavily discussed in the media. While a percentage of people can decrease or eliminate the need for chronic medications through significant lifestyle changes, there have been reports of weight gain in those who stopped taking this injectable medication.
Without intense lifestyle behavior modification education, there is a heightened risk of weight regain in the absence of such medications. Leaders in the treatment of obesity and related illnesses have commented that this drug is intended for long-term use.
Examples of this include the following:
“GLP-1 medications [like Ozempic] are designed to be taken long-term... They are chronic medications for the treatment of chronic conditions (both diabetes and obesity) (12)". - Christopher McGowan, M.D., a gastroenterologist specializing in obesity medicine and endobariatrics
“As with many chronic conditions, most people who use the drugs for diabetes or weight loss will need to keep taking them to keep benefiting from them. Depending on your individual situation, and without sustained lifestyle changes, it is likely you would need to be on these medications indefinitely to maintain weight loss (13)." - Dr. Cecilia Low Wang, a UCHealth expert in endocrinology, diabetes and metabolism.

Self Quiz
Ask yourself...
- Is semaglutide considered to be a long-term treatment for type 2 diabetes?
Cost Concerns
At this time, injectable semaglutide, FDA-approved for the treatment of Type 2 diabetes, has a self-pay price tag of $935.77 per month (4 injections). With FDA approval, many people with diabetes, insured under commercial plans, receive the drug for the cost of their copay. Those patients without coverage may use pharmacy discount cards that reduce the price, on average, to $814.55/month.
The following links are available to familiarize yourself with patient assistance programs related to semaglutide injectables.
Semaglutide Cost Savings Programs
The following links are provided to explore various semaglutide cost savings programs.

Self Quiz
Ask yourself...
- What resources can you offer patients who are struggling to pay for semaglutide?
Emerging Concerns: Semaglutide and gastroparesis
In August 2023, a first-of-its-kind lawsuit was filed in Louisiana, against the makers of semaglutide. The lawsuit states the makers of this injectable drug did not adequately warn patients about the risk of severe gastrointestinal issues/possible gastroparesis.
The plaintiff in this case had used both Ozempic and Mounjaro and experienced repeated episodes of severe gastrointestinal events, warranting trips to the emergency room and additional medications to alleviate her symptoms (14). While this lawsuit is in the developing stages, it bears mentioning in terms of concerns over long-term usage of the drug and possible complications.
While the drug labeling for semaglutide (Ozempic) does not specifically mention gastroparesis, the semaglutide/Mounjaro drug label does state that the drug has not been studied in patients with severe gastrointestinal disease and is therefore not recommended in these patients.
Up to 50% of people with diabetes have some degree of delayed gastric emptying, but most have no digestive symptoms or have only mild symptoms. For some people with diabetes, problems managing blood glucose levels may be a sign of delayed gastric emptying (15).
Healthcare providers should evaluate all patients with diabetes for possible symptoms of underlying gastroparesis, such as the feeling of fullness shortly after beginning a meal, or the inability to finish a regular meal. Other symptoms of gastroparesis may include abdominal pain, nausea, bloating, vomiting, and anorexia.
Diabetes and gastroparesis
Uncontrolled or poorly controlled diabetes can affect nerve endings systemwide. Diabetes is a very common cause of gastroparesis. Although the condition is rare it occurs more often in people with chronic conditions such as diabetes, autoimmune diseases, and nervous system disorders. Nerve endings are injured or damaged, cease to function properly, and result in delayed gastric emptying. The delay in gastric emptying can cause various symptoms, such as nausea, vomiting, bloating and distension, abdominal pain, and poor appetite.
In addition to underlying medical conditions, some medications may cause symptoms of gastroparesis (delays in gastric emptying and overall gastric motility. These medications include narcotics, antidepressants, and anticholinergics.
Left untreated, diabetic gastroparesis may lead to malnutrition, electrolyte imbalances, and poor glucose management and control.

Self Quiz
Ask yourself...
- Why should nurses prescribing semaglutide watch out for symptoms of gastroparesis?
- What do you think are some ethical issues with semaglutide use for weight loss?
Diabetes Lifestyle changes: Patient education (16)
- Weight Management
- Healthy Eating
- Physical Activity
- Smoking Cessation
- Stress Management
The importance of patient education regarding lifestyle changes is a priority. As with any chronic medication condition, the patient and their family/support system must be given every opportunity to educate and empower themselves on self-management of their disease process. Patients must be given the benefit of the doubt that they can indeed embrace their health and well-being and work with their healthcare provider in maximizing their health outcomes.
For diabetes mellitus, numerous lifestyle behaviors should be addressed and actively worked on, so that the patient receives the maximum health benefits. The following lifestyle behaviors are in no particular order; they all warrant discussion at every office visit.
Diet
A person with diabetes should be educated on the effects of food and nutrition on their glucose level. Referrals to a dietitian/nutritionist or Certified Diabetes Care Education Specialist (CDCES) should be considered a top priority. Well-balanced nutritional intake, appropriate carbohydrate awareness, calorie monitoring if weight loss is appropriate to your specific patient) and medication/food interactions are all essential aspects of dietary lifestyle education. Many commercial insurance plans, as well as hospital community outreach programs, offer diabetes self-management classes.

Activity (17)
The CDC recommends a target goal of 150 minutes weekly, Patients should be educated on the positive effects of daily activity on overall health and well-being, stress management, and metabolism. Patients should find activities they are genuinely interested in, involve family and friends, and slowly build greater endurance through increased intervals of longer duration.
Sleep hygiene (18)
Patients should be educated on the positive effects of a good night’s sleep. The aim should be approximately 7-8 hours of restful sleep. Electronics should be powered down and (optimally) removed from the bedroom. A dark, well-vented, cool room temperature is encouraged, and large meals and late-evening caffeine should be avoided.
Medication adherence/ literacy
Medication education is critical to the health and well-being of a patient. Routine education of the patient, and family members or support systems when available, should be supportive and patient-specific. Patients should be assessed on language barriers, literacy issues, and related comprehension concerns. Medication education should include effects, side effects, treatment goals, and sick day management. Emergency care issues should also be discussed. Any monitoring equipment (continuous glucose monitors, accuchecks, lancets) should be reviewed with patients and confirmed with return verbalization and demonstration.
As discussed in this course, patients with chronic diseases must learn self-management techniques to optimize their health and well-being. They must become confident in their understanding of their disease process and take ownership of their health. In doing so, they minimize the risk of long-term complications, improve their self-worth, and actively invest (both time and money) in their future.

Self Quiz
Ask yourself...
- How does sleep, diet, and activity level affect the treatment of type 2 diabetes?
Ozempic Case Study
- 52-year-old female
- Height 67 inches
- Weight 225 pounds
- B/P 138/84, Heart rate 76 NSR
- BMI 35.2%
- Nonsmoker, occasional social drinker
- Multiple attempts at dieting without success.
- Diagnosed T2DM approx. 6 months ago current A1C 7.5%; initial medication Metformin 500mg BID tablets; tolerated well. No GI upsets.
Today’s appointment is for evaluation and additional medication consideration (the patient requested this appointment)
The patient was diagnosed with T2DM approximately 6 months ago. Initial A1C 8.0%. Current A1C 7.7%
Despite an improved diet and adherence to the medication regimen, the patient voiced frustration at the lack of weight loss. Requesting additional medication. Has a neighbor friend who began injectable Ozempic and is having “really great results with it. I want to start on it as well”.
- What are your thoughts on prescribing semaglutide injectable for this patient?
- What objective health data points should be taken into consideration regarding prescribing semaglutide for this patient?
The patient has expressed frustration that despite taking her medications and adjusting her diet, she has not lost any weight in the past 6 months. She has “heard from her neighbor friend that the weight just melts off immediately” and she is ready to start this medication.
- What concerns do you know about this patient's understanding of weight loss as it relates to semaglutide?
- What prescribing information, specific to semaglutide and weight loss, could you share with your patient regarding realistic weight loss targets?
- In addition to teaching your patient proper injection technique for the use of semaglutide, what other lifestyle education behaviors should you discuss at this point?
- What information should you share with your patient regarding the long-term use of semaglutide and the potential risks of stopping this medication (as it relates to weight regain)?
Your patient decides to go ahead with the semaglutide regimen.
- What are some patient education guidelines regarding common side effects of this medication?
- How often is the dose increased? What is the maximum dose this patient can receive weekly?
Your patient wants to know how long she will be taking this medication.
- What talking points will you cover regarding the long-term use of this medication?
- How do you best prepare this patient for long-term success with this medication?
- What lifestyle behavior modification education would you discuss with your patient, to give her the best chance at successfully managing her diabetes?
Medication Assisted Treatment
Introduction
Medication Assisted Treatment (MAT) is a treatment modality for substance use disorders. It combines counseling and behavioral therapies for addiction with medications used carefully to reduce the physical symptoms of cravings and withdrawal and assist clients in the recovery process. With half of people 12 and older reporting use of an illicit substance at least once and 21 million Americans experiencing addiction, this is an important and relevant topic (4).
Historically, an intense stigma is attached to both addiction and some of the medications used to treat addiction. A thorough understanding of substance use disorders, available MAT therapies, and care of affecting clients are essential topics for nurses to be familiar with, particularly those working in psychiatry, pain management, or addiction medicine.
Overview of Addiction and Substance Abuse:
Drug and alcohol abuse and addiction are chronic, complicated issues involving persistent changes to the brain. There is a stigma or misunderstanding that people with substance abuse disorders can stop any time they want to or lack the willpower or moral fortitude to stop using. This is entirely untrue, and even people who are "recovering" and have not had any drugs or alcohol in years can easily relapse into addiction once those brain changes have occurred (5).
When a person uses drugs or alcohol, the brain's reward center is flooded with dopamine. This provides a "buzz" or pleasurable sensation that may create the desire to use more of the same substance. Over time, and with regular use of the substance, the brain becomes accustomed to the flooding of dopamine and reduces the reward response, a process known as tolerance.
It will now take the same person a more significant amount of the substance to achieve the same "buzz" or "high" they used to feel. This process can also dull the pleasure response to activities not involving substance use, such as food, socialization, or sexual activity. Over time, the chemical changes in the brain can progress to include decreased functioning of learning, decision-making, judgment, response to stress, memory, and behavior (5).
To understand substance abuse disorders, it is first essential to understand some basic definitions. These terms are sometimes used interchangeably, but they mean different things and represent different stages of disease.
Definitions
Substance Use: Substance use is any consumption of drugs or alcohol, regardless of frequency or amount. An occasional glass of wine or taking an edible at a party is an example of substance use. Substance use does not cause problems or dependency in many people (5).
Substance Abuse: Substance abuse is the continued use of drugs or alcohol, even when they do cause problems. Conflict or problems at home, school, work, or legal issues related to the use of drugs or alcohol are signs of abuse. For example, being sent home from school for smoking in the bathroom or failing a drug test at work (5).
Substance Dependence or Addiction: Dependence and addiction can be used interchangeably or is sometimes called substance use disorder. Addiction occurs when a person cannot stop drinking or using drugs despite creating problems in their life. People who are addicted may experience cravings until they use a specific substance, or they may experience uncomfortable physical symptoms, known as withdrawal if they do stop (5).
The American Psychiatric Association (APA) utilizes the following criteria to diagnose clients who suffer from addiction. The more criteria a client answers yes to, the greater their problem with substance use.
Six or more positive criteria are indicative of addiction.
- Using substance in more significant amounts or for more extended periods than intended
- Trying to stop using but being unable to
- Increased amounts of time getting, using, or recovering from use of the substance
- Experiencing cravings or urges to use.
- Continuing to use the substance despite problems with relationships or social situations.
- Missing work, social, or recreational obligations or activities because of substance use
- Participating in risky behavior because of substance use
- Continuing to use the substance despite psychological or physical health problems.
- Needing to use more substance over time to achieve the desired effect.
- Experiencing withdrawal symptoms when stopping the substance (1).


Self Quiz
Ask yourself...
- Do you know anyone who suffers from a substance use disorder?
- Think about your biases (thoughts, opinions, attitudes) about addiction. Does any of the information above conflict with those biases?
Substance Abuse Statistics
Many factors go into gathering data on substance abuse disorders, from underreporting, the nuance between use, abuse, and addiction, and the large variety of substances available, with the legality of some substances varying by state or age.
The statistics below from 2020 are not meant to be an exhaustive list of substance use disorders in this country but rather an overview of some of the more prevalent addiction-related issues.
- 50% of people 12 years and older have used an illicit substance at least once.
- 5% of Americans 12 years and older have used drugs within the last month.
- This is a 3.8% increase from the previous year.
- About 50% of Americans 12 and over drink alcohol
- 4% of those people have an alcohol use disorder.
- About 20% of Americans use tobacco products or vape
- 18% of Americans over 18 used marijuana in the last 12 months
- 30% of those have some level of misuse or addiction.
- Marijuana is commonly involved in polysubstance use, paired with alcohol or other drugs.
- 7% of Americans over 12 misused opioids in the last 12 months
- 96% of those used prescription pain relievers
- Opioid prescriptions peaked in 2012, with 81.3 prescriptions per 100 people.
- The rate has declined recently due to increased attention to this crisis.
- In 2018, the rate was down to 51 prescriptions for every 100 people
- Fentanyl is now rising as a new and deadly concern.
- 5 million prescriptions were written for fentanyl in 2015.
- Fentanyl is involved in 53% of overdose deaths.
- 7% of all Americans misuse a prescription drug.
- 1% of those misuse stimulants
- 2% of those misuse sedatives
- 5% misuse painkillers
- Over 70,000 drug overdose deaths occur annually in the United States (4)
Risk Factors
A combination of factors is involved in the risk of addiction, and no one factor can determine if someone will develop addiction or after how many uses this will occur.
The addiction process does occur more easily or progresses more rapidly for people with certain risk factors, including:
Genetics
There is a strong genetic correlation with addiction, indicating that biology plays a significant role in the disorder. Family history of addiction, gender, ethnicity, and comorbid mental health conditions can all influence the risk of addiction. (5)
- Children of addicts are eight times more likely to develop an addiction at some point.
- In 2020, among those using illicit or misusing prescription drugs, 22% were male and 17% female.
- Only 20% of users in drug treatment programs are women.
- 9% of people with substance abuse disorders also have at least one mental health disorder (4)
Environment/Non-Genetic Demographics
The attitudes about drugs and alcohol from those in a person's network and life experiences play a role in the risk of addiction. Substance use among friends, family, or coworkers increases the risk that a person will also use substances. Exposure to substance use from a young age relaxed parental attitudes about substance use, and peer pressure from friends can increase the risk. Certain stressful life circumstances such as veteran status, history of sexual or physical assault, or being part of the LGBTQ community can also increase risk. (5)
- 20% of people in urban areas used illegal drugs in 2020 compared to 5% in rural locations.
- 51% of Americans with an illegal pain relief medication obtained it from a friend or relative.
- 7% of LGBTQ Americans abuse illicit drugs.
- 2% of LGBTQ Americans abuse alcohol.
- 7% of Veterans abuse illicit drugs.
- 80% of Veterans abuse alcohol (4)
Developmental Stage
Substance use at any age can lead to addiction, but children and teens are at particular risk due to their underdeveloped brains. The parts of the brain responsible for decision-making, risk assessment, and self-control do not fully develop until the early 20's, putting teenagers at increased risk of dangerous behaviors. In addition, the effects of drugs and alcohol on the developing brain may mean that those parts of the brain never fully develop at all for teens with substance abuse disorders. (5)
- 70% of users who try an illegal substance before age 13 will develop a substance use disorder within the next seven years.
- This is for only 27% of people who first try an illegal substance after age 17.
- 47% of youths report trying an illegal substance by the time they graduate high school (4)

Self Quiz
Ask yourself...
- Why do you think medication alone is not an adequate treatment for substance abuse disorders?
- Is MAT something you have heard of before? Why do you think it is relatively uncommon despite being around for decades?
Overview of Medication Assisted Treatment (MAT)
Treatment of substance abuse disorders is a complex and often tumultuous process. The nature of the brain changes that occur during addiction means that a person is never entirely "cured" but will always be considered "recovering" as the risk for relapse is always present. Effective treatment must be multifaceted and often involves removing triggers (such as people, places, and stressors) that may prompt a person to use again behavioral therapy, and medications to curb withdrawal symptoms and reduce cravings.
Medication Assisted Treatment (MAT) is a treatment that involves FDA-approved medications, in combination with behavioral therapy, in the recovery process for substance abuse disorders. Several medications are available for MAT, and evidence continues to emerge that the treatment is highly effective if used correctly.
However, it is a vastly underused and understudied treatment modality. MAT has been available in some form for over 50 years but is just starting to gain traction among the medical community (and policymakers) in recent years, with the federal government calling for more research and increased accessibility for the treatment (8).
The height of the opioid crisis in the last several years has highlighted the magnitude of drug addiction and deaths in the United States, bringing renewed attention to MAT as a treatment option. So, how does MAT work? Prescription medication is given to both stimulate the receptors seeking the abused substance and block the drug's euphoric effects.
Over time, this normalizes brain chemistry and helps the person break the habit of using without the discomfort of cravings and withdrawal symptoms. Gradually, the prescription medication dosage is reduced, all the while in conjunction with behavioral therapy and lifestyle changes, and eventually, the client should be able to stop the medication altogether, often within 1-3 months (8).
MAT does require close supervision by a trained medical professional and an appropriate facility for treatment. It can be done on an inpatient, partial inpatient, or outpatient basis. There may be side effects to the medication, and there is a risk of misusing or developing addiction to the new drug, though the successful outcomes often outweigh this risk. Clients must also participate in behavioral therapy for a comprehensive and effective treatment plan. As with any treatment regimen, careful consideration of the client's history and circumstances is essential (8).


Self Quiz
Ask yourself...
- Why do you think medication alone is not an adequate treatment for substance abuse disorders?
- Is Medication Assisted Treatment (MAT) something you have heard of before? Why do you think it is relatively uncommon despite being around for decades?
Pharmacokinetics
Currently, there are three medications with FDA approval for MAT: buprenorphine, methadone, and naltrexone. Each will be discussed in depth below.
Buprenorphine
Mechanism of Action and Metabolism
Buprenorphine is an opioid partial agonist, acting on the same receptors as other opioids but with weaker effects. It can be used for the treatment of misuse of opioids, including:
- Heroin
- Fentanyl
- Oxycodone
- Hydrocodone
- Morphine
- Methadone (3)
Opiate receptors are G-protein coupled receptors (GPCRs) with four major types: Mu, Delta, Kappa, and opioid receptor like-1 (ORL1). Stimulation of these receptors results in varying levels of the following effects:
- Euphoria
- Relaxation
- Pain relief
- Sleepiness
- Sweating
- Constipation
- Impaired concentration
- Reduced sex drive (3)
Buprenorphine has a high affinity to the Mu-opioid receptor and is a partial agonist at this site, causing reduced opioid effects with a plateau or ceiling at higher doses. This limits dangerous effects and makes overdose unlikely. It also has slow dissociation from the site, allowing milder and more easily tolerated withdrawal effects compared to full agonists like morphine and fentanyl. Buprenorphine is also a weak kappa receptor antagonist and delta receptor agonist, reducing the craving sensation and improving tolerance to stress (3).
Buprenorphine has poor bioavailability when given orally due to the first-pass effect, where most of the drug is broken down in the liver and intestines. Because of this, sublingual or buccal are the preferred routes of administration and the most common forms in which the drug is manufactured. Transdermal patches and IV and IM forms exist, though not for use in MAT (3).
CYP34A enzymes break down buprenorphine, so other drugs, such as ketoconazole, may inhibit metabolism and increase available levels of buprenorphine. CYP34A inducers such as carbamazepine, topiramate, phenytoin, and barbiturates may speed metabolism and lower available levels. Once broken down, the med takes the form of norbuprenorphine and is excreted in the feces (3).
Available Forms
Buprenorphine is available by itself and with naloxone (in a 4 to 1 ratio). However, in oral form, naloxone is not readily absorbed, and buprenorphine is the only genuinely active ingredient. This combination is beneficial should clients try to inject their buprenorphine to get high; naloxone is a fast-acting opioid antagonist that is active when used intravenously and would block the opioid effect of buprenorphine, rendering it useless for recreational use and ensuring it has no street value.
The currently available preparations of buprenorphine for MAT include:
- Generic Buprenorphine/naloxone sublingual tablets
- Subutex - Buprenorphine sublingual tablets
- Suboxone - Buprenorphine/naloxone sublingual films
- Zubsolv - Buprenorphine/naloxone sublingual tablets
- Bunavail - Buprenorphine/naloxone buccal film (3)
Sublingual products dissolve within 2-10 minutes. Bloodstream absorption begins quickly, bypassing the first pass effect. Buprenorphine has a slow onset of action, peaking about 3-4 hours later. Metabolism is also slow, with the half-life lasting anywhere from 25 to 70 hours (an average of about 38 hours). This long half-life means the drug can be spaced out to every other day administration once weaning begins (3).
Dosing and Monitoring
Clients prescribed buprenorphine must stop using opioids for at least 12 to 24 hours before the first dose; this varies depending on which opioid they are stopping. For short-acting opioids like heroin and oxycodone, buprenorphine may be started 6-12 hours after the last dose. With longer-acting opioids such as morphine or extended-release preparations of oxycodone, buprenorphine should be delayed for about 24 hours. For the longest action opioids, fentanyl patch, 48 -72 hours must be between the last dose and buprenorphine initiation (3).
This initiation schedule means clients will be in the early stages of discomfort and withdrawal. Administration of buprenorphine when clients still have opioids in their bloodstream will lead to competition for receptor sites, rapidly replacing the opioid with buprenorphine and causing acute and more severe withdrawal symptoms.
Depending on the severity of a client's addiction, they may complete the first step of abstaining and withdrawal in an inpatient setting. Once the initial withdrawal symptoms have passed and the initial dose of buprenorphine has been given, the client may be discharged home to continue buprenorphine initiation on an outpatient basis (3).
Initial doses are typically 2-4mg, with up to 4mg given to clients used to higher potency or larger doses of opioids. The dose is gradually increased to meet the client's individual needs, with a maximum dosage of 24mg per day. The average client requires 8-12 mg per day and can reach this dose within the first 2-4 days. It is recommended that doses be supervised by a pharmacist at the dispensing pharmacy for the first two months of treatment to ensure compliance and clients are less likely to relapse (3).
The length of treatment with buprenorphine depends on each client's case and, for some, may be indefinite. Clients who do wish to wean off buprenorphine can begin the process once they are stable and experiencing few or no cravings, and a minimum of 8 weeks from treatment initiation. Doses are moved to alternating days and eventually discontinued altogether (3).
Side Effects and Contraindications:
As with any medication, there are potential side effects, including:
Common Side Effects
- Nausea
- Vomiting
- Drowsiness
- Dizziness
- Headache
- Memory loss
- Sweating
- Dry mouth
- Miosis
- Postural hypotension
- Sexual dysfunction
- Urinary retention
Serious side effects
- CNS depression
- QT prolongation
- Reduced seizure threshold
- Potential for abuse or overdose (3)
Buprenorphine is contraindicated for clients with a past hypersensitive reaction to it. It should be used cautiously for clients with respiratory suppression, older adults, or for those with liver pathologies. Regular monitoring of liver enzymes via lab work is essential (3).
It is a Category C medication for pregnancy, and the risks versus benefits should be carefully weighed. Buprenorphine does cross the placenta and increases the risk of withdrawal symptoms and neonatal abstinence syndrome (NAS) after delivery. However, for pregnant clients with the highest risk of relapse and abuse of opioids, evidence does support that continuation of buprenorphine during pregnancy may improve maternal and fetal outcomes (3).
Buprenorphine may be abused by crushing tablets, snorting the powder, or dissolving it into an injectable solution. Safety measures against this include supervised administration by a pharmacist and the addition of naloxone, which blocks the buprenorphine effects. While the effect ceiling of buprenorphine makes overdose difficult, combining the drug with benzodiazepines, alcohol, or other drugs can compound the CNS depressant effects and increase the risk of overdose (3).
Clinicians need to have a comprehensive health history of clients before initiating buprenorphine so that all risks and potential interactions can be addressed appropriately.
Role of the Pharmacist
Pharmacists play a significant role in the success of MAT involving buprenorphine. Outpatient doses are monitored by the dispensing pharmacist daily, with at-home quantities being allowed on a limited basis (such as weekends or travel) and only for the most motivated and compliant clients. Vital signs are collected before each dosage, with careful monitoring for hypotension or bradypnea. The dose may be skipped for clients who experience excessive side effects, and the client can return the next day for their dose.
Clients presenting with signs of overdose (usually to the ED) may receive naloxone, which will reverse overdose symptoms within 1 hour. Overdose symptoms include dizziness, pinpoint pupils, hypotension, bradypnea, hallucinations, seizure, or unconscious state.
If a client misses a dose, does not show up for it, or is experiencing significant side effects from buprenorphine, the prescribing clinician should be notified so that the treatment plan can be revisited and revised if needed (3).
Considerations for the Prescriber
When considering which medication to prescribe for MAT, prescribers should understand that buprenorphine offers advantages over methadone.
- Lower risk of abuse
- Safer, including at higher doses.
- Therapeutic dose achieved quickly.
- Easier to taper.
- Can be obtained from any provider rather than a methadone clinic.
- Less stigma
The cost of a 30-day supply is around $300. Buprenorphine/naloxone combinations are a little more expensive at $400/month. While prior authorization is usually required, most commercial insurance and state Medicaid programs will cover the medication.
Buprenorphine is a Schedule III Controlled Substance; however, recent federal regulations have been aimed at approving access to MAT, and any provider with an active DEA license may prescribe buprenorphine as allowed by state regulations. Specialized clinics are not required (as they are with methadone), and it is dispensed at regular pharmacies.
Prescribers are encouraged to participate in additional training about MAT with buprenorphine, but it is not required. Detailed documentation must be completed, including the reason for prescribing, start and end dates of treatment, the pharmacy used, the credentials of who will supervise administration, and frequency of follow-up and compliance monitoring. The sublingual and buccal routes are the only forms of medication used for MAT; patches, IM, and IV preparations are not routinely used for MAT.
The success of buprenorphine treatment depends on the client's education. Addiction potential, risk of combination with other CNS depressants, and side effects vs. signs of overdose should all be discussed with clients and their support system (3).

Self Quiz
Ask yourself...
- Given the nature of substance abuse disorders, why do you think including an opioid antagonist like naloxone in preparations of buprenorphine is necessary for safety and compliance?
- What challenges do you see with a medication needing to be administered daily with pharmacist supervision?
- What are the risks of buprenorphine being given without this supervision?
- Consider the possible pros and cons of taking a medication like buprenorphine during pregnancy. Also, consider the risks of NOT taking the drug during pregnancy when a substance use disorder is present.
Methadone
Mechanism of Action and Metabolism
Methadone is a synthetic opioid and a full agonist of the Mu-receptor site, stimulating the same effects as opioids.
- Euphoria
- Analgesia
- Sedation
It can be used as a potent analgesic for pain not responding to traditional medications, such as in clients with cancer or terminal illness, as well as for MAT and neonatal abstinence syndrome (NAS).
For this course, it will be discussed as a MAT agent, used in treatment for clients addicted to opioids such as:
- Heroin
- Fentanyl
- Oxycodone
- Hydrocodone
- Morphine
- Hydromorphone (2)
Methadone is a full agonist at the Mu-receptor, meaning it is a more potent and more easily addictive medication than partial agonists like buprenorphine. Methadone has a long half-life (8-60 hours), occupying the Mu-receptors and blocking short-acting opioids from making a client high. The longer half-life also leads to less severe cravings and withdrawal symptoms. Methadone is also an antagonist to the N-methyl-d-aspartate (NMDA) receptor, which adds to its pain relief action (2).
It has high oral bioavailability, is active in the bloodstream within 30 minutes of ingestion and remains elevated for around 24 hours. It is broken down via CYP3A4 and CYP2B6 enzymes and metabolized through the liver, making it a good option for clients with renal problems.
Medications such as ciprofloxacin, benzodiazepines, fluconazole, cimetidine, and fluoxetine may slow methadone metabolism, increasing the available drug and the side effects of overdose risk. Other medications may speed metabolism and decrease the effects of methadone, including phenobarbital, phenytoin, rifampin, ritonavir, and carbamazepine (2).
Available Forms
Methadone is available in many forms, including oral, IM, subcutaneous, IV, and intrathecal, though only the oral is typically used for MAT.
- Methadone - tablets
- DISKETS - dispersible/dissolvable tablet
- Methadone HCL Intensol - 10mg/ml suspension
- Methadone - dispersible tablet (2)
Dosing and Monitoring
Oral dosing is initiated at 30-40 mg/day with a slow titration of 10-20 mg/week until the optimal dosage is reached. The optimal dosage varies by client and depends on the drug they are replacing, tolerance to opioids, and side effects experienced. A dosage between 80- 150 mg/day is the typical goal. (2)
If parenteral methadone is given, it is usually 50%-80% of the oral dosage.
Blood sugar, EKG, and methadone blood levels should be checked regularly, every week for higher-risk patients, and every 3-6 months for those in good health and compliance. The target methadone blood level is around 400 ug/ml (2).
Side Effects and Contraindications
Potential side effects are directly related to stimulation of the opioid receptors and include:
- Diaphoresis
- Flushing
- Pruritus
- Nausea
- Dry mouth
- Constipation
- Sedation
- Lethargy
- Respiratory Depression
- QT prolongation
- Hypoglycemia (2)
Methadone should be considered with a comprehensive view of a client's health history and other medications. Clients with CNS-related disease processes (trauma, increased ICP, dementia, or delirium) must be monitored closely or have other medication considered.
Methadone should not be used simultaneously as other opioids, benzodiazepines, alcohol, or antipsychotics due to increased CNS effects. Methadone is a Pregnancy Category C medication, and risks versus benefits should be weighed carefully. Infants exposed to methadone in utero are at increased risk of NAS after delivery (2).
Overdose can occur, and clients and support systems should be educated on signs of overdose.
- Lethargy
- Somnolence
- Stupor
- Coma
- Miosis
- Bradycardia
- Hypotension
- Respiratory sedation
- Cardiac arrest
Naloxone is used to reverse overdose (2).
Considerations for Prescribers and Clinics
Methadone is a Schedule II Controlled Substance, meaning it has a high abuse potential and must be carefully monitored. The Prescription Drug Monitoring Program (PDMP) is an electronic database used nationwide to register the distribution of controlled substances so that clients do not seek care at multiple clinics or pharmacies to obtain more of a controlled substance.
When prescribing methadone, providers should check the PDMP for both methadone and other prescription opioids so that they are fully aware of other medications clients may be receiving from other places. Regular urine drug screening should be performed to make sure clients are not using other substances not obtained by prescription and that they are testing positive for methadone, meaning they are genuinely taking it if administration is not observed (2).
At the beginning of treatment, methadone is given in the office under a nurse's supervision, and then clients are monitored for adverse effects. Some take-home doses (up to 7 in the first two weeks) may be arranged for weekends or during travel, but this possibility is limited during the first few weeks of treatment. As treatment progresses and compliance is demonstrated, clients may self-administer more doses at home (up to 28 doses per month) and go longer between visits to the clinic. The total length of treatment varies but is often 1-2 years and can even be indefinite (7).
There are methadone clinics that work entirely in the scope of addiction management, but primary care providers may prescribe methadone as well. Prescribers must have an active DEA license and comply with state-based controlled substance regulations (2).


Self Quiz
Ask yourself...
- Why do you think methadone is a Schedule II Controlled Substance while buprenorphine is only a Schedule III?
- What are the benefits of checking the serum level of methadone?
- What might the clinical presentation be for someone overdosing on methadone?
- Have you ever used the PDMP database before? What are the benefits of accessing this database?
Naltrexone
Mechanism of Action and Metabolism
Naltrexone has been in use since the 1960s and is an opioid antagonist. It competes primarily with the mu-receptor but also serves as an antagonist at the kappa and delta receptors. As an antagonist, it competes with agonists such as opioids and alcohol and blocks the effects of agonists at those sites.
- Prevents euphoria.
- Prevents intoxication.
- Reduces tolerance (6)
Naltrexone also acts on the hypothalamic-pituitary-adrenal axis, modifying it to reduce cravings and suppress alcohol consumption.
It is FDA-approved for use in clinical practice for the treatment of:
- Alcohol use disorder
- Opioid use disorder (prescription and non)
Naltrexone is absorbed orally and undergoes extensive metabolism via the first-pass effect. However, this does not affect its potency as naltrexone's active metabolite, 6β-naltrexone, acts as a potent opioid antagonist. The medication's half-life is around 4 hours but can last up to 24 hours. If administered parenterally, it bypasses the first pass and is even longer acting, with a half-life of 5-10 days. Naltrexone is excreted by the kidneys (6).
Available Forms
Naltrexone is available in an oral tablet and IM injection. Available preparations include:
- Generic naltrexone tablets
- Revia (oral tablet)
- Depade (oral tablet)
- Vivitrol (solution for IM injection, extended-release) (6)
Dosing and Monitoring
Since naltrexone will compete for and block all opioid receptor sites, the risk for withdrawal symptoms is high, and clients must stop the use of alcohol or opioids for 7-10 days before beginning treatment to lessen the risk of withdrawal symptoms. A naltrexone challenge is recommended at the start of therapy.
This consists of administering small amounts of naltrexone subcutaneously or via IV and monitoring the client and their vital signs for signs of withdrawal, such as:
- Nausea
- Vomiting
- Diaphoresis
- BP changes
- Tachycardia
- Rhinorrhea
- Agitation
- Tremors
- Abdominal pain
- Pupillary dilation (6)
If a client fails the naltrexone challenge and has not been long enough since their last use of alcohol or opioids, the naltrexone initiation should be delayed, and the test should be repeated in 24 hours. If clients tolerate the naltrexone test and the negative result, they may begin naltrexone treatment (6).
For oral tablets, dosing usually starts at 25 mg for the first dose. Clients are observed for withdrawal symptoms and side effects; an additional 25 mg is given 1 hour later. After that, clients take 50 mg per day. Clients may continue with 50mg daily or take 100 mg every other day or 150 mg every 3rd day (6).
Alternatively, naltrexone may be given via IM injection for more extended action, improving compliance and reducing relapse. Particularly for alcohol or heroin dependence, data indicates that the IM route has much higher success rates than the oral route. If a client receives the IM injection, 380 mg is given to the gluteal muscle every four weeks (6).
Side Effects and Contraindications
Most common side effects of naltrexone include:
- GI irritation
- Diarrhea
- Abdominal cramps
- Nausea
- Vomiting
- Hypertension
- Headache
- Anxiety
- Low energy
- Joint or muscle pain
- Nervousness
- Sleep disruption
Less commonly, clients report:
- Loss of appetite
- Constipation
- Dizziness
- Irritability
- Depression
- Rash
- Chills (6)
Caution should be used for clients with liver function issues and renal impairment. It is Category C for use during pregnancy, and the risks versus benefits of use in pregnancy must be carefully considered. It also crosses into breast milk and must be considered carefully.
There is limited data about the overdose of naltrexone, and there may be very few symptoms if an overdose occurs. Clients should be monitored for signs of liver dysfunction, seizures, depression, and suicidal ideations. No antidote for naltrexone is currently available.
Naltrexone is contraindicated for clients who failed a naltrexone challenge, test positive for opioids or alcohol on drug screening, have a history of seizures, or have experienced a past hypersensitivity reaction to naltrexone.
Clients may switch from buprenorphine or methadone to naltrexone at some point in treatment. Both medications are agonists at the opioid receptor sites, so changing to naltrexone (an antagonist) may increase the risk of withdrawal symptoms for the first two weeks of treatment (6).
Considerations for Prescribers
Because naltrexone does not cause any euphoria or "high," the abuse potential is non-existent. It is not a controlled substance and can be prescribed by any clinician with prescriptive authority. However, its use is typically only by those who work in mental health or addiction medicine. Clients can take the medication at home or go to the clinic for IM injections.
Many considerations for naltrexone use center around monitoring for side effects and treatment compliance. Baseline and periodic drug screening and liver function tests are prudent. Clients' support persons should be educated on compliance and signs of relapse. The IM formulation should be considered for those with poor compliance or most at risk for relapse (6).

Self Quiz
Ask yourself...
- Why might a client benefit from the IM formulation of naltrexone instead of the oral preparation?
- Why might compliance with an opioid antagonist be more complex than an opioid agonist like methadone or buprenorphine?
- How do side effects differ between naltrexone and the agonist medications like methadone?
- What does it mean if a client fails a "naltrexone challenge," and how does this delay their care?
Nursing Considerations
Nurses will encounter clients with addiction and even those receiving MAT in a variety of settings, including:
- Outpatient clinics for routine care of any health issues
- ED admission for acute problems not related to addiction.
- Inpatient hospitalization related to other health problems.
- Outpatient setting for participation in MAT or addiction management.
- ED admission for acute problems related to substance abuse or toxicity of MAT medication.
- Inpatient mental health admission for mental health and addiction issues
Regardless of the setting and if the client is being seen for an addiction issue or something else, it is crucial for nurses to be familiar with MAT medications and how they work to provide safe and competent care. Nurses may need to:
- Administer medication.
- Monitor lab results.
- Observe for side effects, toxicity, or withdrawal symptoms.
- Coordinate care within a multidisciplinary team
- Communicate with therapeutic and nonjudgmental techniques.


Self Quiz
Ask yourself...
- Have you ever cared for a client in a non-addiction setting who had a MAT medication on their drug list?
- Did you have any biases or preconceived ideas about what this medication meant?
- Is there anything you have learned throughout this course that will change your care the next time you encounter a client receiving MAT?
Case Study
Justin is a 32-year-old male who presents to the ED with nausea, lethargy, and confusion worsening over the last 24 hours. Upon exam, the nurse notes diaphoresis, slurred speech, and pinpoint pupils. His vitals are RR 10, HR 54, BP 82/58, SPO2 97%, Temp 99.0.
He reports taking Wellbutrin 150mg daily for depression and smoking cessation, methadone 100mg daily for history of oxycodone abuse, and was started on ciprofloxacin 250mg BID for a UTI 2 days ago at urgent care.
His labs are significant for a WBC of 15,000 but otherwise regular. He tests positive for methadone, which is expected, but not for other substances. He reports being compliant with MAT and avoiding opioid use for nine months.
It is determined that Justin is experiencing methadone toxicity due to the slowed metabolism of the drug from the combination of methadone and ciprofloxacin. He is given naloxone in the ED, and within an hour, his symptoms have improved significantly, and his vital signs are typical. His antibiotic is switched to cefdinir, and he is discharged home in stable condition with instructions to follow up with his PCP within 1-2 days.

Self Quiz
Ask yourself...
- Given Justin's presentation, how could you differentiate between methadone toxicity and relapse?
- How might Justin's condition have progressed if he had not sought emergency care?
- How would Justin's case have been different if he had not tested positive for methadone?
- In what ways could Justin's care before his ED visit have been improved to avoid this complication?
Conclusion
Substance use disorders are a long-standing and dangerous pathology experienced by millions of people each year. At the same time, the stigma of seeking help for such disorders has been eroding in recent years; there has also been a renewed push by the federal government to address the issue in evidence-based and meaningful ways, with access to effective treatment being at the top of the priority list.
Addiction treatment programs utilizing MAT will likely become much more popular in the coming years, and nurses will be on the front lines of this therapy. For nurses to provide competent and comprehensive care to this client population, up-to-date and accurate knowledge is necessary.
Hypertensive Agents
Definitions
Hypertension – high blood pressure above normal. Normal is considered anything less than 120/80 mmHg [7].
Antihypertensives – medications used to control hypertension and lower blood pressure [7].
Hypertensive crisis – severely elevated blood pressure of either:
- Systolic greater than 180 mmHg
- Diastolic greater than 120 mmHg [19].
Hypertensive emergency – acutely elevated blood pressure with signs of target organ damage [2].
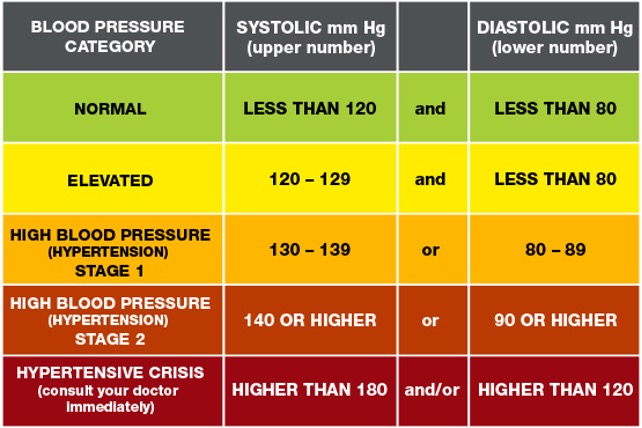

Self Quiz
Ask yourself...
- What is hypertension?
- What are antihypertensives?
- What is a hypertensive crisis?
- What is a hypertensive emergency?
Medications Overview
Antihypertensive medications are used for the treatment of hypertension and are used in both inpatient, outpatient, and emergency settings.
Some of the major antihypertensive medication classes include:
- Diuretics
- Beta-blockers
- Angiotensin-converting enzyme inhibitors
- Angiotensin II receptor blockers
- Calcium channel blockers
- Selective alpha-1 blockers
- Alpha-2 Receptor Agonists
- Vasodilators [3].
Different medical organizations have varying recommendations and hypertension treatment guidelines. Hypertension treatment clinical practice guidelines are available from organizations like the American Heart Association, the American College of Cardiology, and the European Society of Cardiology to name a few [21]. Healthcare providers should be aware of their healthcare institution’s recommendations for clinical practice guidelines and organizations.
All organizational guidelines share the same recommended treatment of starting antihypertensives immediately when:
- Blood pressure is greater than 140/90 mmHg for patients with a history of ischemic heart disease, heart failure, or cerebrovascular disease.
- Blood pressure is greater than 160/100 mmHg regardless of underlying medical conditions [21].
Again, healthcare providers should follow current and evidence-based clinical guidelines for initiating or titrating antihypertensive medications.
While most antihypertensives are prescribed in an outpatient setting, certain antihypertensives are indicated during hypertensive or medical emergencies. For example, intravenous (IV) vasodilators, like nitroprusside and nitroglycerin, and calcium channel blockers, like nicardipine, are used during hypertensive emergencies and crises.


Self Quiz
Ask yourself...
- In what settings are antihypertensives used?
- What are the clinical guidelines for initiating hypertensive medications?
- Which medications are commonly used to treat hypertensive emergencies?
Pharmacokinetics
Diuretics
Diuretics are a class of drugs that help control blood pressure by removing excess sodium and water from the body through the kidneys. There are several varying types of diuretics, some including thiazide, potassium-sparing, and loop, and all work to lower blood pressure differently [3].
Thiazide Diuretics
Thiazide diuretics remove excess sodium and water from the body by blocking the sodium-chloride (Na-Cl) channels in the kidneys’ distal convoluted tubule. As the Na-Cl channel becomes blocked, this inhibits the reabsorption of sodium and water into the kidneys. Concurrently, this causes a loss of potassium and calcium ions through the sodium-calcium channels and sodium-potassium pump [1].
Thiazide diuretics are approved by the Food and Drug Administration (FDA) for controlling primary hypertension and are available via oral route. Some common thiazide diuretics are hydrochlorothiazide, chlorthalidone, and metolazone [3].
When initiating this medication, the healthcare provider should start with the lowest dose, which is usually 25mg daily, and then increase accordingly to aid with blood pressure control or if the patient has excess fluid retention, usually as evidenced by leg swelling or edema [1].
Common side effects of thiazide diuretics include:
- Increased urination
- Diarrhea
- Headache
- Stomach and muscle aches [16].
As thiazide diuretics interfere with Na-Cl, Na-Ca, and Na-K channels, there is an increased potential for adverse effects, including:
- Hypotension
- Hypokalemia
- Hyponatremia
- Hypercalcemia
- Hyperglycemia
- Hyperlipidemia
- Hyperuricemia
- Acute pancreatitis
When prescribing thiazide diuretics, healthcare providers should avoid prescribing thiazide diuretics to patients with a sulfonamide allergy, since thiazides are sulfa-containing medications. Also, they should avoid prescribing these to patients with a history of gout [1].
Additionally, patients can experience a thiazide overdose if they take more than the amount prescribed. Patients with a suspected overdose may experience confusion, dizziness, hypotension, and other symptoms. These patients must seek emergency care and poison control must be alerted [16].
Potassium-Sparing Diuretics
Potassium-sparing diuretics remove excess sodium and water from the body without causing loss of potassium. Depending on the type, they interrupt sodium reabsorption by either binding to epithelial sodium channels or inhibiting aldosterone receptors. When catatonic sodium is reabsorbed, this creates a negative gradient causing the reabsorption of potassium ions through the mineralocorticoid receptor [5].
Potassium-sparing diuretics are approved for controlling hypertension and are usually combined with other diuretics, like thiazide or loop diuretics since they have a weak antihypertensive effect.
Common names of potassium-sparing diuretics are amiloride, triamterene, and spironolactone. These medications are available by either intravenous or oral routes. Spironolactone is commonly used for treating primary aldosteronism and heart failure [5]. Patients should be started on the lowest dose when first prescribing this class of medications.
Common side effects can include:
- Increased urination
- Hyperkalemia
- Metabolic acidosis
- Nausea
[4]
Healthcare providers should avoid prescribing this class of medications to patients with hyperkalemia or chronic kidney disease. They should also be avoided during pregnancy or in patients who are taking digoxin. Since potassium-sparing medications can cause hyperkalemia, periodic monitoring for electrolyte imbalances and potassium levels is necessary [4].
Loop Diuretics
Loop diuretics inhibit sodium and chloride reabsorption by competing with chloride binding in the Na-K-2Cl (NKCC2) cotransporter. Potassium is not reabsorbed by the kidney, which causes additional calcium and magnesium ion loss.
Loop diuretics are FDA-approved for the treatment of hypertension but are not considered first-line treatment. They can also be used for treating fluid overload in conditions like heart failure or nephrotic syndrome [12].
Loop diuretics are available via oral or IV routes and furosemide, torsemide, and bumetanide are common forms [3].
Bioavailability and dosage differ for each type and route of loop diuretics. The bioavailability of furosemide is 50%, with a half-life of around 2 hours for patients with normal kidney function, and dosages start at 8mg for oral medication. Torsemide has a bioavailability of about 80%, a half-life of about 3 to 4 hours, and oral dosages start at 5mg [12].
Common side effects can include:
- Dizziness
- Increased urination
- Headache
- Stomach upset
- Hyponatremia
- Hypokalemia [13].
Loop diuretics can lead to several adverse effects, including toxicity, electrolyte imbalances, hyperglycemia, and ototoxicity. They have a black box warning stating that high dosages can cause severe diuresis. Therefore, electrolytes, BUN, and creatinine values should be monitored closely by a healthcare provider.
People with a sulfonamide allergy may also be allergic to loop diuretics, so this should be avoided if the patient is allergic. Loop diuretics also interfere with digoxin and therefore should be avoided. Other contraindications include anuria, hepatic impairments, and use during severe electrolyte disturbances [12].


Self Quiz
Ask yourself...
- What is the pharmacokinetics of thiazide diuretics?
- What is the pharmacokinetics of loop diuretics?
- What is the pharmacokinetics of potassium-sparing diuretics?
- What are common side effects and contraindications for each type of diuretic?
Beta-Blockers
Beta-blockers work by reducing the body’s heart rate and thus, lowering cardiac output resulting in lowered blood pressure [3]. The mechanism of action for beta-blockers varies, depending on the receptor type it blocks, and are classified as either non-selective or beta-1 (B1) selective.
Non-selective beta-blockers bind to the B1 and B2 receptors, blocking epinephrine and norepinephrine, causing a slowed heart rate. Propranolol, labetalol, and carvedilol are common non-selective beta-blockers.
Alternatively, beta-1 selective blockers only bind to the B1 receptors of the heart, so they are considered cardio-selective. Some examples include atenolol, metoprolol, and bisoprolol. Sotalol is a type of beta-blocker that also blocks potassium channels and is, therefore, a class III antiarrhythmic [8].
Beta-blockers are not primarily used for the initial treatment of hypertension but can be prescribed for conditions like tachycardia, myocardial infarction, congestive heart failure, and cardiac arrhythmias. It’s also approved for use in conditions such as essential tremors, hyperthyroidism, glaucoma, and prevention of migraines.
Beta-blockers are available in many forms, including oral, IV, intramuscular injection, and ophthalmic drops. Starting dosage and route are determined by the health condition being treated [8].
Common side effects of beta-blockers include:
- Bradycardia
- Hypotension
- Dizziness
- Feeling tired
- Nausea
- Dry mouth
- Sexual Dysfunction
[17]
This class of medications can also lead to more severe adverse effects such as orthostatic hypotension, bronchospasm, shortness of breath, hyperglycemia, and increased risk of QT prolongation, torsades de pointes, and heart block [8]. Healthcare providers should avoid prescribing non-selective beta-blockers to patients with asthma. Instead, they can prescribe cardio-selective beta-blockers for patients with asthma.
Additionally, the use of beta-blockers is contraindicated in patients with a history of bradycardia, hypotension, Raynaud disease, QT prolongation, or torsades de pointes. Healthcare providers must encourage patients to monitor their heart rate and blood pressure and follow administration parameters before taking beta-blockers daily since it decreases their heart rate.
Overdose of beta-blockers is life-threatening and healthcare providers must discuss the symptoms of an overdose and the need for emergency care [8].

Self Quiz
Ask yourself...
- What is the pharmacokinetics of beta-blockers?
- What are the common side effects and contraindications of beta-blockers?
Angiotensin-converting Enzyme Inhibitors
Angiotensin-converting enzyme (ACE) inhibitors prevent the body from producing angiotensin, a hormone that causes vasoconstriction. As angiotensin production is reduced, this allows the blood vessels to dilate and therefore lowers blood pressure [3].
Moreover, ACE inhibitors act specifically on the renin-angiotensin-aldosterone system (RAAS) by preventing the conversion of angiotensin I to angiotensin II. It also works to decrease aldosterone, which in turn, decreases sodium and water reabsorption [9].
ACE inhibitors usually end in the suffix -pril and some common examples include lisinopril, benazepril, enalapril, and captopril, and they usually end in the suffix [3].
While ACE inhibitors are approved for treating hypertension, they are also FDA-approved for other uses or combination therapies for medical conditions such as:
- Systolic heart failure
- Chronic kidney disease
- ST-elevated myocardial infarction
One non-approved FDA use is treatment of diabetic nephropathy [9]. This class of medication is available in oral, and IV forms, and dosages are dependent on clinical guidelines, underlying medical conditions, and route.
ACE inhibitors have common side effects, with some including:
- Dry cough
- Dizziness
- Hypotension [9].
This medication can also lead to adverse effects, such as syncope, angioedema, and hyperkalemia [9]. As angioedema is an adverse effect, healthcare providers should understand this class of medications is contraindicated in patients with a history of hypersensitivity to ACE inhibitors.
Additionally, ACE inhibitors are contraindicated in patients with aortic valve stenosis, hypovolemia, and during pregnancy. Individuals with abnormal kidney function should have renal function and electrolyte values monitored. If a patient develops a chronic dry cough, then the healthcare provider should consider another antihypertensive medication class by following current guidelines [9].

Self Quiz
Ask yourself...
- What is the pharmacokinetics of angiotensin-converting enzyme inhibitors?
- What are common side effects and contraindications of angiotensin-converting enzyme inhibitors?
Angiotensin II Receptor Blockers
Similar to ACE inhibitors, Angiotensin II Receptor Blockers (ARBs) act on the RAAS by binding to angiotensin II receptors and thus block and reduce the action of angiotensin II. Again, this reduces blood pressure by causing blood vessel dilation and decreasing sodium and water reabsorption [11]. ARBs typically end in the suffix -artan and common names are losartan, valsartan, and Olmesartan [3]. Oral and IV routes of the medication are available and again, dosages are dependent on the medication specifically and form [11].
All ARBs are FDA-approved for the treatment of hypertension, but a select few are approved for treating other medical conditions, such as:
- Candesartan for heart failure
- Irbesartan for diabetic nephropathy
- Losartan for proteinuria and diabetic nephropathy
- Telmisartan for stroke and myocardial infarction prevention
- Valsartan for heart failure and reduction of mortality in patients with left ventricular dysfunction [11].
Although not as common as ACE inhibitors, two side effects of ARBs are dry cough and angioedema.
Other common side effects include:
- Dizziness
- Hypotension
- Hyperkalemia
[11]
Contraindications for use are if the patient is pregnant or has renal impairment or failure. If a patient is on an ARB, the healthcare provider should closely monitor lab values for electrolyte imbalances and kidney function.
Additionally, if a patient is taking lithium, ARBs can increase lithium concentration and therefore, lithium blood concentration should be frequently checked [11].

Self Quiz
Ask yourself...
- What is the pharmacokinetics of angiotensin II receptor blockers?
- What are common side effects and contraindications of angiotensin II receptor blockers?
Calcium Channel Blockers
Calcium channel blockers (CCBs), also known as calcium channel antagonists, act by preventing calcium from entering the smooth vascular and heart muscles. In turn, this reduces heart rate and causes vasodilation [3].
They are further divided into two major categories, non-dihydropyridines and dihydropyridines, where there are differences in the mechanism of action. Non-dihydropyridines inhibit calcium from entering the heart’s sinoatrial and atrioventricular nodes and thus cause a cardiac conduction delay and reduce cardiac contractility.
Alternatively, dihydropyridines do not directly affect the heart but do act as a peripheral vasodilator leading to lowered blood pressure. Both categories are metabolized by the CYP3A4 pathway [15].
Names of non-dihydropyridine CCBs are verapamil and diltiazem. Dihydropyridine CCBs typically end in the suffix -pine and common names are amlodipine and nicardipine. Both categories are available via oral and IV routes for administration. Oral dosages of non-dihydropyridine CCBs start at 30mg daily and dihydropyridine CCBs start at 30mg daily for immediate release [15].
Calcium channel blockers can be used to treat other medical conditions in addition to hypertension and include:
- Coronary spasm
- Angina pectoris
- Supraventricular dysrhythmias
- Pulmonary hypertension
- Hypertrophic cardiomyopathy
Non-dihydropyridine CCBs can cause side effects like bradycardia, and constipation, while dihydropyridine CCBs can cause:
- Headaches
- Feeling lightheaded
- Leg swelling [15].
Both categories pose the risk of potential hypotension and bradycardia, so healthcare providers should closely monitor the patient’s blood pressure and heart rate when initiating or titrating the dosage.
Also, an overdose of this medication can lead to cardiac conduction delays, complete heart block, and cardiovascular collapse. Patients with possible symptoms of overdose should be sent to the emergency room immediately.
Additionally, healthcare providers should avoid prescribing CCBs to people with heart failure and sick sinus syndrome [15].

Self Quiz
Ask yourself...
- What is the pharmacokinetics of calcium channel blockers?
- What are the common side effects and contraindications of calcium channel blockers?
Selective Alpha-1 Blockers
Selective alpha-1 blockers act on the body’s sympathetic nervous system to lower blood pressure. They prevent norepinephrine from binding to the alpha-1 receptors of the sympathetic nervous system, causing smooth muscle relaxation and vasodilation which leads to lowered blood pressure [18].
Selective alpha-1 blockers are available via the oral route, end in the suffix -osin and examples are doxazosin, terazosin, and prazosin [3]. They are FDA-approved for the treatment of hypertension but are not considered first-line therapy. Additionally, this class of medications may be used to treat benign prostatic hyperplasia. Dosages can start as low as 1mg daily depending on the drug selected.
Common side effects include:
- Hypotension
- Tachycardia
- Dizziness
- Headache
- Weakness [18].
As selective alpha-1 blockers can lead to orthostatic hypotension, the healthcare provider should instruct the patient to take this medication at night. They should also avoid prescribing to the elderly population when able because of hypotension and increased fall risk [18].

Self Quiz
Ask yourself...
- What is the pharmacokinetics of alpha-1 blockers?
- What are the common side effects and contraindications of alpha-1 blockers?
Alpha-2 Receptor Agonists
Alpha-2 receptor agonists work by decreasing the activity of the sympathetic nervous system to lower blood pressure. It inhibits adenylyl cyclase and decreases the formation of cyclic adenosine monophosphate (cAMP). Alpha-2 agonists also cause vasodilation by reducing the amount of available cytoplasmic calcium [20].
This class of medications is typically administered via oral route but is also available in intravenous and transdermal forms. Two FDA-approved alpha-2 agonists for hypertension treatment are methyldopa and clonidine and dosages are dependent on the name and route.
Methyldopa is commonly prescribed to patients with hypertension and who are pregnant since it’s safe [20].
Common side effects of alpha-2 receptor agonists are:
- Dry mouth
- Drowsiness
- Fatigue
- Headache
- Sexual dysfunction [3].
Contraindications for use are orthostatic hypotension and autonomic disorders. Healthcare providers must avoid prescribing alpha-2 receptor agonists to individuals taking phosphodiesterase inhibitors [20].

Self Quiz
Ask yourself...
- What is the pharmacokinetics of alpha-2 receptor agonists?
- What are common side effects and contraindications of alpha-2 receptor agonists?
Vasodilators
Vasodilators lower blood pressure by dilating the body’s blood vessels. It binds to the receptors of the blood vessel’s endothelial cells, releasing calcium. Calcium stimulates nitric oxide synthase (NO synthase), eventually converting to L-arginine to nitric oxide. As nitric oxide is available, this allows for GTP to convert to cGMP, and causes dephosphorylation of the myosin and actin filaments. As this occurs, the blood vessels’ smooth muscles relax, leading to vasodilation and lowered blood pressure.
Common vasodilators that act via this pathway are nitrates and minoxidil. Hydralazine is another vasodilator, but the mechanism of action is unknown [10].
Available forms of vasodilators are sublingual, oral, and intravenous. Similar to other classes of antihypertensives, vasodilator dosages depend on the form and treatment setting [10].
Nitrovasodilators like nitroprusside and nitroglycerin are used during hypertensive emergencies. Hydralazine is used for severe hypertension for the prevention of eclampsia or intracranial hemorrhage and minoxidil for resistant hypertension [10] [3].
Side effects for each will vary, but nitrates commonly cause:
- Reflex tachycardia
- Headache
- Orthostatic hypotension
[10]
Common side effects of hydralazine are headaches, heart palpitations, and myalgias. Minoxidil causes excessive hair growth, weight gain, and fluid retention [3]. Additionally, nitroprusside can potentially cause cyanide toxicity.
Vasodilators have varying degrees of contraindications, such as nitrates are avoided in patients with an inferior myocardial infarction. Hydralazine should not be given to patients with coronary artery disease, angina, or rheumatic heart disease. Healthcare providers should be aware of contraindications and monitor patients’ blood pressure and potential side effects [10].

Self Quiz
Ask yourself...
- What is the pharmacokinetics of vasodilators?
- What are the common side effects and contraindications of vasodilators?
Combination Antihypertensives
Many antihypertensive medications come in combined forms, such as ACE inhibitors and thiazide diuretics, beta-blockers and diuretics, or calcium channel blockers and ACE inhibitors. The mechanism of action for combination antihypertensives depends on the blend of medications [3].
Considerations for Prescribers
This section reviews potential considerations when prescribing antihypertensives.
When prescribing antihypertensive medications, there are several factors that healthcare providers must consider. The route is typically determined by the healthcare setting and dosage by the underlying treatment goals. Again, healthcare providers should follow current guidelines when initiating or titrating antihypertensive medications.
Healthcare providers must complete a thorough health history, and review lab values, and contraindications as mentioned above. Monitoring kidney function and electrolyte values is imperative while any patient is taking antihypertensive medications.
While a single antihypertensive medication is recommended for initial treatment, there are some scenarios where combination therapy or combination antihypertensives are recommended [14].
Healthcare providers should also discuss the potential side effects of antihypertensives with patients and what to do if they are experiencing symptoms. For instance, if a patient reports syncope, they should be advised to go to the emergency room or be seen immediately for further evaluation. Also, healthcare providers must encourage patients to monitor their heart rate and blood pressure at home and abide by administration parameters.
For example, instruct patients who are taking beta-blockers to measure their blood pressure and heart rate before taking their medication. If their heart rate is below 60 beats per minute, then they should not take the medication [14].
If a patient is experiencing side effects from an antihypertensive medication, then another alternative should be selected.


Self Quiz
Ask yourself...
- What factors should healthcare providers consider when prescribing antihypertensives?
Upcoming Research
This section reviews upcoming research and medications for hypertension treatment.
Research on antihypertensive medications has slowed throughout the years. Some clinical trials were performed on the potential of endothelin receptor antagonists to reduce hypertension. However, some studies found several unwanted side effects, and thus clinical use was stopped for safety reasons.
An endothelin-A and endothelin-B receptor blocker, called aprocinentan, has shown promise for the treatment of resistant hypertension by lowering blood pressure and decreasing vascular resistance.
Research on sodium-glucose transport protein (SGLT2) inhibitors, which are typically used for the treatment of type II diabetes mellitus, is also ongoing. SGLT2 inhibitors may promote blood pressure reduction through diuresis and reduce sympathetic tone [21].

Self Quiz
Ask yourself...
- What new research is there about antihypertensives?
Conclusion
If hypertension is left untreated, it can lead to serious health complications, including death. When selecting antihypertensive treatment, healthcare providers should understand the pharmacokinetics of each drug class along with potential side effects and contraindications. They should also follow current clinical guidelines for an evidence-based approach.
Final Reflection Questions
- Which antihypertensive medication is often prescribed during pregnancy?
- Which lab values are important when monitoring patients on each antihypertensive medication?
- Which antihypertensive medications cause hypokalemia?
- Which antihypertensive medications cause hyperkalemia?
Migraine Management

Self Quiz
Ask yourself...
- How might a comprehensive knowledge of migraine medications, including their mechanisms of action, enhance the ability of healthcare professionals to address the specific needs of patients experiencing migraines?
- In what ways can recognizing warnings related to migraine medications contribute to ensuring patient safety?
Definition
Migraines are recurrent, pulsating headaches often accompanied by other symptoms such as nausea, sensitivity to light, and sensitivity to sound. According to recent studies by (17), migraines are recognized as a complex neurological disorder involving abnormal brain activity and a cascade of events leading to pain and associated symptoms.
The impact of migraines extends beyond physical pain, influencing various aspects of life, and recent literature by (14) highlights the profound effect on the quality of life, with disruptions in daily activities, work, and social interactions. For example, a professional experiencing frequent migraines might struggle to meet work deadlines and engage in social events. Recent advancements in diagnostic criteria by (15) emphasize the importance of a precise definition to ensure appropriate treatment strategies. Therefore, understanding the definition is crucial for accurate diagnosis and effective communication between healthcare providers and patients.


Self Quiz
Ask yourself...
- What distinguishes migraines from common headaches, and how does understanding this difference impact the approach to their management?
- In what ways do migraines extend beyond physical pain, and how might this impact influence an individual's overall quality of life?
- How can a precise definition of migraines contribute to accurate diagnosis, and why is accurate diagnosis essential for effective treatment planning?
- How does understanding the definition of migraines facilitate effective communication between healthcare professionals and patients?
Migraine Medications
Understanding the various classes of migraine medications is like having a diverse toolkit to address the complexities of this neurological disorder. By exploring the different classes of medications, healthcare professionals can tailor their approach and make informed decisions based on individual patient profiles and specific migraine characteristics (20).
It is crucial to recognize that migraine medications are not one-size-fits-all. Each patient is unique, and their response to medications may vary. Recent literature by (12) emphasizes the importance of an individualized approach when considering the best medication for each patient. Here’s a list of migraine medications in addition to important details to consider:
Triptans
Triptans are a class of medications specifically designed for the acute treatment of migraines. According to (39), they are not meant for preventive use but are highly effective in providing relief during an ongoing migraine attack. They work by narrowing blood vessels and inhibiting the release of certain chemicals in the brain associated with migraine symptoms (39). Let’s see more details below as described by (7), (39), (29).
Drug Class
Belonging to the serotonin (5-HT) receptor agonists class, Triptans modulate the effects of serotonin receptors in the brain. The various types of Triptans include Sumatriptan, Rizatriptan, Eletriptan, and others. Each Triptan has unique characteristics, such as the onset of action and duration, allowing healthcare professionals to tailor prescriptions based on individual patient needs.
Benefits
Triptans offer several benefits in the management of migraines. One of the primary advantages is their ability to provide rapid and effective relief from migraine symptoms, including headache pain, nausea, and sensitivity to light and sound. The prompt onset of action is particularly valuable for individuals aiming to resume their daily activities quickly. Triptans are available in various formulations, including oral tablets, nasal sprays, and injectables, allowing for flexibility in administration.
Side Effects
While generally well-tolerated, Triptans may cause side effects. Common side effects include mild sensations of warmth or tingling, dizziness, and tightness or pressure in the chest. It is crucial for healthcare professionals to consider the patient's medical history and potential contraindications, such as cardiovascular issues, before prescribing Triptans. In rare cases, more severe side effects like chest pain and changes in heart rate may occur, necessitating immediate medical attention.
Clinical Effects
The clinical effects of Triptans are profound, offering relief to individuals experiencing acute migraine attacks. The primary outcomes include:
- Pain Relief: Triptans are highly effective in reducing the intensity of migraine-associated pain. By targeting the vascular and neuronal components of migraines, these drugs provide rapid relief, allowing patients to resume their normal activities.
- Relief of Associated Symptoms: Beyond pain relief, Triptans address accompanying symptoms such as nausea, photophobia, and phonophobia. This comprehensive effect enhances the overall patient experience during a migraine episode.
- Prevention of Migraine Progression: Triptans, when administered early in the migraine attack, can prevent the progression of the headache phase to more severe stages. This early intervention is crucial for optimizing outcomes and minimizing the impact of migraines on daily life.
- Improvement in Functional Impairment: Migraines often result in functional impairment, limiting individuals' ability to perform daily tasks. Triptans restore functional capacity, allowing patients to regain control over their activities.
Nonsteroidal Anti-Inflammatory Drugs (NSAIDSs)
Nonsteroidal anti-inflammatory drugs, commonly known as NSAIDs, constitute a class of medications used in the treatment of migraines. According to (6), these drugs are characterized by their anti-inflammatory, analgesic, and antipyretic properties. NSAIDs are versatile, as they are not exclusively used for migraines but are also used for various other pain and inflammatory conditions (6). Let’s see more details below as described by (25), (40), (6) and (28).
Drug Class
NSAIDs encompass a broad class of medications, including well-known examples such as ibuprofen, naproxen, and aspirin. They function by inhibiting enzymes called cyclooxygenases (COX), thereby reducing the production of inflammatory prostaglandins. This mechanism provides relief from pain and mitigates inflammation associated with migraines.
Benefits
The primary benefit of NSAIDs in migraine management lies in their ability to alleviate pain and reduce inflammation. They are particularly effective for individuals experiencing mild to moderate migraines. NSAIDs offer a rapid onset of action, making them suitable for individuals seeking prompt relief. Additionally, these medications are available over-the-counter in many formulations, providing accessibility for patients.
Side Effects
While NSAIDs are generally well-tolerated, they may cause side effects, especially with prolonged or excessive use. Common side effects include gastrointestinal issues such as stomach upset or ulcers. Healthcare professionals need to consider a patient's medical history, including conditions like gastric ulcers, before prescribing NSAIDs. In rare cases, more severe side effects like cardiovascular events may occur, emphasizing the importance of cautious use.
Clinical Effects
The clinical effects of NSAIDs in migraine management encompass various aspects. Here’s a list of some of them.
- Pain Relief: NSAIDs are effective in providing pain relief during acute migraine attacks. By reducing prostaglandin levels, they alleviate headache symptoms and contribute to the overall comfort of individuals experiencing migraines.
- Inhibition of Inflammatory Responses: The anti-inflammatory properties of NSAIDs are particularly beneficial when migraines are associated with inflammatory processes. NSAIDs help mitigate inflammation, reducing the severity and duration of migraine attacks.
- Improvement in Associated Symptoms: Beyond pain relief, NSAIDs address associated symptoms such as nausea and photophobia, enhancing the overall patient experience during a migraine episode.
- Prevention of Migraine Progression: When administered early in the migraine attack, NSAIDs can prevent the progression of headaches to more severe stages. This early intervention is critical for optimizing outcomes and minimizing the impact of migraines on daily life.
Calcitonin Gene-Related Peptide (CGRP) Inhibitors
Calcitonin gene-related peptide (CGRP) inhibitors represent a modern class of medications revolutionizing the landscape of migraine management. According to (11), these drugs specifically target CGRP, a neuropeptide involved in dilating blood vessels and transmitting pain signals. By inhibiting CGRP, these inhibitors aim to modulate migraine pathways and reduce the frequency and severity of attacks (11). Let’s see more details below as described by (23) and (11).
Drug Class
CGRP inhibitors belong to a unique drug class designed explicitly for migraine prevention. Examples of CGRP inhibitors include Erenumab, Fremanezumab, and Galcanezumab. These medications are administered via subcutaneous injections, typically monthly or quarterly. The focus on preventive therapy distinguishes CGRP inhibitors from acute treatment options like Triptans.
Benefits
The primary benefit of CGRP inhibitors lies in their efficacy in preventing migraines. Clinical trials have demonstrated a significant reduction in the frequency of monthly migraine attacks among individuals using CGRP inhibitors. This preventive approach is especially valuable for those with frequent and debilitating migraines, offering a chance to enhance their quality of life.
Moreover, CGRP inhibitors are well-tolerated with fewer side effects than other preventive medications. They provide a targeted and specific intervention, addressing the underlying mechanisms of migraines without causing widespread effects on other bodily functions.
Side Effects
While generally well-tolerated, CGRP inhibitors may have some side effects. Local injection site reactions, such as redness or swelling, are common but typically mild. It is crucial for healthcare professionals to monitor and address any adverse effects promptly. Additionally, ongoing research is essential to further understand the long-term safety profile of these medications.
Clinical Effects
The clinical effects of CGRP inhibitors are transformative in the realm of migraine management, offering a novel approach to prevention. Primary clinical effects include the following:
- Reduction in Migraine Frequency: One of the hallmark effects of CGRP inhibitors is a significant reduction in the frequency of migraine attacks. By consistently blocking CGRP receptors, these medications disrupt the migraine cascade, leading to a sustained preventive effect.
- Improvement in Migraine Severity: CGRP inhibitors not only reduce the frequency but also contribute to a decrease in the severity of migraine attacks. This comprehensive effect enhances the overall quality of life for individuals suffering from chronic migraines.
- Enhanced Functional Capacity: Migraines often result in functional impairment, limiting individuals' ability to perform daily tasks. CGRP inhibitors restore functional capacity, allowing patients to regain control over their activities and participate more fully in their daily lives.
- Well-Tolerated Profile: CGRP inhibitors are generally well-tolerated, with a favorable side effect profile. This characteristic enhances patient adherence to preventive treatment, a critical factor in long-term migraine management.
Beta-Blockers
Beta-blockers are a class of medications that have found a significant place in migraine management. Initially developed for cardiovascular conditions, beta-blockers have demonstrated efficacy in preventing migraines by reducing the frequency and severity of attacks (32). According to (32), these medications work by blocking the effects of adrenaline, leading to reduced heart rate and blood pressure. Let’s see more details below as described by (32) and (27).
Drug Class
Beta-blockers encompass various medications, with examples such as propranolol, metoprolol, and timolol commonly prescribed for migraine prevention. These drugs fall into the broader category of antihypertensive medications but are repurposed for their preventive benefits in migraine care. Unlike acute treatments, which provide relief during an ongoing attack, beta-blockers are taken regularly to reduce the overall occurrence of migraines.
Benefits
The primary benefit of beta-blockers in migraine management is their preventive action. Clinical studies have shown that beta-blockers can significantly reduce the frequency of migraines, making them particularly suitable for individuals with chronic or frequent attacks. This preventive approach aims to enhance the overall quality of life for those who experience migraines regularly.
Beta-blockers are especially beneficial for individuals with comorbid conditions such as hypertension or heart disease. By addressing both cardiovascular concerns and migraines, these medications offer a comprehensive therapeutic approach.
Side Effects
While generally well-tolerated, beta-blockers may cause side effects that individuals need to be aware of. Common side effects include fatigue, dizziness, and changes in sleep patterns. Healthcare professionals need to monitor patients regularly and adjust the dosage or consider alternative medications if side effects become problematic. Beta-blockers are typically avoided in individuals with certain heart conditions, emphasizing the importance of an individualized approach.
Clinical Effects
The clinical effects of beta-blockers in migraine management encompass various dimensions. See some examples below:
- Reduction in Migraine Frequency: Beta-blockers are known for their ability to reduce the frequency of migraine attacks significantly. This preventive effect is especially valuable for individuals experiencing chronic migraines, enhancing their overall quality of life.
- Alleviation of Migraine Severity: Beyond frequency reduction, beta-blockers contribute to a decrease in the severity of migraine attacks. This comprehensive effect enhances the overall comfort of individuals during migraine episodes.
- Improvement in Associated Symptoms: Beta-blockers have been shown to address associated symptoms such as nausea and sensitivity to light. By modulating the autonomic nervous system, these medications offer a holistic approach to migraine management.
- Cardiovascular Benefits: Beta-blockers provide additional benefits for individuals with comorbidities due to their primary use in cardiovascular conditions. This dual action allows for comprehensive management of both migraine and cardiovascular health.
Anticonvulsants
Anticonvulsants, originally developed to control seizures in epilepsy, have emerged as a valuable class of medications in the preventive management of migraines (9). According to (9), these drugs, also known as antiepileptic drugs (AEDs), work by stabilizing electrical activity in the brain and reducing the frequency and severity of migraine attacks. Let’s see more details below as described by (32) and (9).
Drug Class
Anticonvulsants comprise a diverse class of medications, including Topiramate, Valproic acid, and Gabapentin. While their primary use may be in epilepsy, the preventive benefits of certain anticonvulsants extend to migraines. These medications are taken regularly to provide ongoing protection against migraines.
Benefits
The primary benefit of anticonvulsants in migraine management is their preventive action. Clinical trials have demonstrated the efficacy of certain anticonvulsants, such as topiramate, in significantly reducing the frequency of migraines. This preventative approach is particularly suitable for individuals with chronic or frequent attacks, aiming to improve overall quality of life.
Anticonvulsants are especially valuable for individuals who may not find relief or experience intolerable side effects with other preventive medications. The versatility of this drug class allows healthcare professionals to tailor treatment plans based on individual patient characteristics and responses.
Side Effects
While generally well-tolerated, anticonvulsants may cause side effects that individuals need to be aware of. Common side effects include drowsiness, dizziness, and gastrointestinal disturbances. It is crucial for healthcare professionals to monitor patients regularly and adjust the dosage or consider alternative medications if side effects become problematic. Additionally, certain anticonvulsants may have specific considerations, such as the need to regularly monitor liver function in individuals taking Valproic acid.
Clinical Effects
The clinical effects of anticonvulsants in migraine management encompass the following dimensions:
- Reduction in Migraine Frequency: Anticonvulsants are known for their ability to significantly reduce the frequency of migraine attacks. This preventive effect is particularly valuable for individuals experiencing chronic migraines, substantially improving their overall quality of life.
- Alleviation of Migraine Severity: Beyond frequency reduction, anticonvulsants contribute to a decrease in the severity of migraine attacks. This comprehensive effect enhances the overall comfort of individuals during migraine episodes.
- Improvement in Associated Symptoms: By modulating neurotransmission and neuronal excitability, Anticonvulsants address associated symptoms such as nausea and sensitivity to light. This holistic approach contributes to a more comprehensive management of migraines.
- Beneficial in Comorbid Conditions: Anticonvulsants, due to their broader neurological effects, can be helpful for individuals with comorbid conditions such as epilepsy or mood disorders. This dual benefit allows for comprehensive management and improves overall well-being.

Self Quiz
Ask yourself...
- How do Triptans contribute to migraine management, and in what scenarios might healthcare professionals prioritize their use during acute migraine attacks?
- Can you differentiate the mechanisms of action between NSAIDs and Triptans in migraine management, and how might this understanding influence the choice of medication for a specific patient?
- What roles do CGRP inhibitors play in migraine pharmacotherapy?
- Consider a scenario where a patient experiences migraines with comorbid cardiovascular issues. How might the choice of medication be influenced by the need to prioritize both migraine relief and cardiovascular safety?
Clinical Criteria for Prescribing
In migraine management, prescribing medications involves a comprehensive understanding of clinical criteria to tailor interventions effectively. This section explores the clinical factors guiding the prescription of migraine medications and the decision-making process for healthcare providers. Here are some of the factors.
Frequency and Severity of Migraine Attacks
An essential consideration in prescribing migraine medications is the frequency and severity of migraine attacks experienced by the patient. For instance, a patient suffering from frequent and severe attacks may benefit from preventive medications to reduce the overall frequency and intensity of migraines (31).
Individual Response to Pain and Associated Symptoms
The subjective experience of pain and associated symptoms during migraines varies among individuals. A patient who experiences intense nausea and vomiting may require medications with rapid onset and alternative formulations, such as nasal sprays or injectables, to address these specific symptoms effectively (8).
Impact on Daily Functioning and Quality of Life
Prescribing migraine medications involves considering the impact of migraines on a patient's daily functioning and overall quality of life (24). For example, a working professional with migraines that significantly impede productivity may require acute medications with fast-acting formulations for quick relief during work hours.
Comorbid Conditions and Patient Preferences
Comorbid conditions and patient preferences are pivotal factors in prescribing migraine medications. A patient with comorbid cardiovascular issues may require careful consideration of medication options to mitigate potential risks (2).

Self Quiz
Ask yourself...
- How does a patient's medical history, especially factors like cardiovascular health, influence the clinical criteria for prescribing migraine medications?
- Why is it essential for healthcare professionals to assess the frequency and severity of migraine attacks when determining the clinical criteria for prescribing medications?
- How do patient preferences contribute to the clinical criteria for prescribing migraine medications?
Pharmacokinetics
Understanding the pharmacokinetics of migraine management medications enables healthcare professionals to tailor treatment plans based on individual patient characteristics, ensuring maximum therapeutic benefit. Let’s get into more details for each of the medications listed above:
Triptans
Absorption
Triptans exhibit distinct pharmacokinetic properties that influence their efficacy and onset of action. Following oral administration, Triptans are absorbed through the gastrointestinal tract and the rate of absorption varies among different Triptans, contributing to differences in their clinical profiles. (39)
Distribution
Upon absorption, Triptans undergo distribution to reach target sites in the body, primarily the central nervous system. Their lipophilic nature allows them to penetrate the blood-brain barrier, enabling interaction with serotonin receptors implicated in migraine pathophysiology. The distribution of Triptans influences their ability to exert effects centrally and peripherally. (39)
Metabolism
Metabolism is a crucial aspect of triptan pharmacokinetics, occurring predominantly in the liver. The enzyme responsible for triptan metabolism is monoamine oxidase-A (MAO-A). (39)
Excretion
The final phase in the pharmacokinetic journey of Triptans is excretion, primarily through renal and biliary routes. Renal excretion eliminates the unchanged drug and its metabolites, while biliary excretion expels metabolites via the bile into the gastrointestinal tract. The interplay between metabolism and excretion contributes to the overall pharmacokinetic profile of Triptans. Variations in renal function may influence the elimination of the half-life of certain Triptans, impacting the duration of their therapeutic effect. (39)
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
Absorption
Following oral administration, NSAIDs are absorbed in the gastrointestinal tract, with the rate and extent varying among different agents. For instance, ibuprofen exhibits rapid absorption, making it suitable for prompt relief during acute migraine attacks. On the other hand, naproxen has a longer duration of action due to slower absorption, making it well-suited for sustained pain relief. (28)
Distribution
Upon absorption, NSAIDs embark on a journey of distribution throughout the body. Their lipophilic nature allows for penetration into various tissues, including inflamed areas. The distribution influences the drug's ability to reach target sites, such as the central nervous system, where NSAIDs exert their analgesic and anti-inflammatory effects. This property is particularly relevant in the context of migraines, where the inflammatory component contributes to pain. (28)
Metabolism
Metabolism plays a role in shaping the pharmacokinetic profile of NSAIDs, occurring primarily in the liver. Enzymes such as cytochrome P450 contribute to the biotransformation of NSAIDs into metabolites. The metabolism of NSAIDs can vary among individuals, impacting factors such as drug efficacy and potential side effects. For example, the metabolism of certain NSAIDs, like diclofenac, can be influenced by genetic polymorphisms, contributing to interindividual variability in drug response. (21)
Excretion
The final phase of the NSAID journey involves excretion, predominantly through the kidneys. Unchanged NSAIDs and their metabolites are eliminated via urine. Considerations of renal function are crucial in the context of NSAID use, as impaired kidney function can lead to prolonged drug half-life and increased risk of adverse effects. Regular monitoring of renal function is essential, especially in individuals with conditions that may affect kidney health. (21)
Calcitonin Gene-Related Peptide (CGRP)
Absorption
Administered via subcutaneous injections, CGRP inhibitors such as Erenumab and Fremanezumab enter the bloodstream directly, allowing for precise control over drug levels. This mode of administration ensures a reliable and consistent absorption rate, contributing to the predictability of therapeutic outcomes. (11)
Distribution
Following absorption, CGRP inhibitors are distributed throughout the body, focusing on target sites implicated in migraine pathophysiology, like the central nervous system. (11)
Metabolism
Unlike many traditional medications, CGRP inhibitors follow a different path in terms of metabolism. Due to their biotechnological origin as monoclonal antibodies, these drugs do not undergo significant hepatic metabolism. Instead, proteolytic enzymes break them down into smaller peptides and amino acids, which occur systemically. This unique metabolic pathway aligns with the specificity of CGRP inhibitors, minimizing interactions with hepatic enzymes and potential drug-drug interactions. (37)
Excretion
The final phase of the CGRP inhibitor journey involves excretion, primarily through the kidneys via renal clearance. This aspect is particularly relevant when considering individual patient factors such as renal function, as impaired kidney function can affect the clearance of CGRP inhibitors and influence their duration of action. (37)
Beta-Blockers
Absorption
Administered orally, beta-blockers like propranolol and metoprolol are absorbed through the gastrointestinal tract. Depending on the condition of the gastrointestinal tract, the rate and extent of absorption can vary, impacting the time it takes for these medications to reach therapeutic levels in the bloodstream. (27)
Distribution
Once absorbed, beta-blockers embark on distribution throughout the body. Their lipophilic nature enables penetration through cell membranes, allowing them to reach target tissues, including the heart and blood vessels. In the context of migraine management, the distribution properties of beta-blockers are crucial for their ability to modulate the autonomic nervous system centrally and peripherally, leading to the desired preventive effects against migraines. (27)
Metabolism
The metabolism of beta-blockers occurs primarily in the liver, where enzymes play a role in their biotransformation. Genetic polymorphisms in these enzymes can contribute to interindividual variability in drug metabolism. (27)
Excretion
The final phase of the beta-blocker journey involves excretion, predominantly through the kidneys, where unchanged beta-blockers and their metabolites are eliminated via urine. The renal excretion of these drugs is relevant when considering individual patient factors, such as renal function, as impaired kidney function can affect the clearance of beta-blockers and influence their duration of action. (27)
Anticonvulsants
Absorption
Typically administered orally, anticonvulsants like topiramate and valproic acid are absorbed through the gastrointestinal tract. The rate and extent of absorption play a crucial role in determining the onset of action and overall effectiveness. (9)
Distribution
Following absorption, anticonvulsants undergo distribution throughout the body. Their lipophilic nature allows them to penetrate the blood-brain barrier, reaching target sites in the central nervous system relevant to migraine pathophysiology. The distribution properties of anticonvulsants contribute to their ability to modulate neuronal excitability centrally and exert preventive effects against migraines. (9)
Metabolism
Metabolism is a crucial aspect of anticonvulsant pharmacokinetics. This occurs predominantly in the liver and enzymes play an important role in the biotransformation of anticonvulsants into metabolites. The metabolism of anticonvulsants can vary among individuals, impacting factors such as drug efficacy and potential side effects. For example, valproic acid undergoes extensive hepatic metabolism, and variations in enzyme activity can lead to interindividual variability in drug response. (30)
Excretion
The final phase in the anticonvulsant journey involves excretion, primarily through the kidneys. Unchanged anticonvulsants and their metabolites are eliminated via urine. This renal excretion is relevant when considering individual patient factors such as renal function, as impaired kidney function can affect the clearance of anticonvulsants and influence their duration of action. (30)

Self Quiz
Ask yourself...
- How do the pharmacokinetics of Triptans, specifically their absorption and distribution, contribute to their efficacy in managing acute migraine attacks?
- Can you explain the key pharmacokinetic parameters of nonsteroidal anti-inflammatory drugs (NSAIDs) used in migraine management and how they influence drug effectiveness?
- What role do pharmacokinetic factors play in the onset and duration of action of calcitonin gene-related peptide (CGRP) inhibitors?
- In the context of migraine medications, how does the pharmacokinetics of beta-blockers influence their absorption, distribution, metabolism, and excretion in the body?
Warnings Related to Migraine Medications
Understanding potential warnings related to migraine medications is essential for healthcare professionals to ensure safe and effective treatment. Here are some factors to consider.
Medication Safety
Migraine medications, whether preventive or acute, come with specific warnings that need careful attention. For instance, some medications may have contraindications for individuals with certain medical conditions or those taking specific medications concurrently. According to (34), healthcare providers must be vigilant in assessing patient medical histories to identify potential contraindications.
Addressing Cardiovascular Risks
Certain migraine medications, such as Triptans, may pose cardiovascular risks, especially in individuals with pre-existing cardiovascular conditions (35). Therefore, it is crucial for healthcare providers to assess patients' cardiovascular health and consider alternative medications or dose adjustments for those at higher risk. For example, a patient with a history of myocardial infarction may be advised to avoid Triptans, and a different class of medication, like NSAIDs, may be recommended.
Pregnancy and Lactation Considerations
Warnings related to pregnancy and lactation are paramount. Some migraine medications may have potential risks during pregnancy, and healthcare providers must carefully weigh the benefits and risks when prescribing for pregnant or lactating individuals. For instance, valproic acid is associated with an increased risk of congenital disabilities, and alternative medications with a safer profile may be preferred for pregnant individuals seeking migraine relief (1).
Managing Medication Overuse Headaches (MOH)
A significant warning associated with migraine medications is the risk of medication overuse headaches (34). To prevent this problem, healthcare providers need to educate patients about the importance of adhering to prescribed dosages and avoiding excessive use of acute medications. Offering alternative strategies, such as lifestyle modifications and preventive medications, can be crucial in managing and preventing MOH.


Self Quiz
Ask yourself...
- What are some common warnings associated with the use of Triptans in migraine management, and how should healthcare providers address these warnings?
- Can you identify specific cardiovascular risks associated with certain migraine medications, and what should be considered when prescribing these medications to patients with pre-existing cardiovascular conditions?
- What warnings are typically associated with the use of valproic acid in migraine management, particularly concerning specific patient populations such as pregnant individuals?
- How do healthcare providers manage and educate patients about the risk of medication overuse headaches associated with certain migraine medications, and what preventive measures can be implemented to minimize this risk?
Alternatives to Migraine Medications
According to (5), integrating alternative methods provides additional tools for healthcare professionals and empowers individuals seeking a more comprehensive and personalized approach to migraine care. Here are some alternative approaches:
Holistic Lifestyle Modifications
Holistic management of migraines involves lifestyle modifications that can significantly impact the frequency and severity of attacks. For instance, incorporating regular physical activity, maintaining a consistent sleep schedule, and managing stress through practices like mindfulness and yoga have shown promise in reducing migraine occurrence (5). Educating patients about these lifestyle changes empowers them to actively participate in their migraine management.
Biofeedback and Relaxation Techniques
Biofeedback and relaxation techniques offer non-pharmacological interventions that enhance self-awareness and control over physiological responses (22). These approaches teach individuals to recognize and manage stress triggers, ultimately reducing the frequency of migraines. For example, biofeedback training that monitors muscle tension and provides real-time feedback can effectively prevent migraines (22).
Acupuncture and Acupressure
According to (22), traditional Chinese medicine practices like acupuncture and acupressure have gained recognition for their potential in migraine management. Acupuncture involves the insertion of thin needles into specific points on the body, while acupressure applies pressure to these points. Research suggests that these methods reduce the frequency and intensity of migraines, providing an alternative avenue for individuals seeking non-pharmacological options (22).
Nutritional Approaches
Dietary modifications and nutritional approaches also play a role in holistic migraine management. For example, identifying and avoiding potential trigger foods, such as those containing tyramine or artificial additives, can be beneficial (10). Additionally, ensuring adequate hydration and incorporating anti-inflammatory foods into the diet may contribute to overall well-being and migraine prevention (10).

Self Quiz
Ask yourself...
- What benefits do biofeedback and relaxation techniques offer in reducing the frequency and intensity of migraines?
- How can biofeedback and relaxation techniques be integrated into a comprehensive migraine management plan?
- What role do dietary modifications and nutritional approaches play in the holistic management of migraines?
- How can healthcare professionals guide patients in identifying trigger foods and making informed nutritional choices?
Nursing Considerations
Nurses play a pivotal role in the holistic care of individuals with migraines, contributing to both the preventive and acute aspects of management through various considerations. Here are some important considerations.
Assessment and Patient Education
A thorough assessment includes evaluating the frequency, duration, and severity of migraines and identifying triggers and associated symptoms (3). Additionally, nurses play a key role in patient education, ensuring individuals clearly understand their migraine condition, the prescribed medications, and potential side effects. For instance, educating a patient about the importance of early intervention with acute medications during a migraine attack empowers them to take timely action.
Monitoring and Adverse Event Management
Nurses actively monitor individuals undergoing migraine treatment, monitoring the response to medications and any potential adverse events. Regular monitoring includes assessing the effectiveness of preventive measures, tracking the frequency of migraine attacks, and identifying patterns that may require adjustments in the treatment plan (34). If adverse events or side effects occur, nurses are instrumental in managing them promptly, collaborating with healthcare providers to ensure the safety and well-being of individuals.
Supportive Care and Holistic Approach
Nursing considerations extend beyond medication management to supportive care and a holistic approach. Nurses provide emotional support, helping individuals cope with the impact of migraines on their daily lives. Moreover, they collaborate with other healthcare professionals to integrate holistic approaches such as lifestyle modifications, stress management, and alternative therapies into the overall care plan. According to (34), this collaborative and patient-centered approach enhances the effectiveness of migraine management.
Documentation and Communication
Accurate and thorough documentation of relevant patient information, medication administration details, and responses to treatment is a fundamental nursing responsibility in migraine management (34). In addition to that, clear and concise communication between nursing staff, healthcare providers, and other healthcare team members ensures continuity of care (34).

Self Quiz
Ask yourself...
- How can a thorough patient assessment contribute to the safe and effective administration of migraine medications?
- How do nursing responsibilities extend beyond medication administration to encompass patient education?
- When monitoring individuals undergoing migraine treatment, what are the essential aspects that nurses should observe?
- How does the collaborative communication between nursing staff, healthcare providers, and other team members contribute to the continuity of care in migraine management?
Upcoming Research
Staying ahead of the curve is essential for healthcare professionals to provide cutting-edge care and optimize outcomes for individuals with migraines. Upcoming research include the following:
Advancements in Targeted Therapies
Recent research has unveiled promising advancements in targeted therapies for migraine management. For example, research about monoclonal antibodies targeting the calcitonin gene-related peptide (CGRP) pathway is proving to be effective in preventing migraines (12).
Digital Health and Telemedicine in Migraine Care
Integrating digital health technologies and telemedicine is a burgeoning trend in migraine management research. Smartphone applications for tracking migraine patterns, wearable devices for monitoring physiological parameters, and virtual consultations enable a more comprehensive and patient-centric approach (12). This shift toward digital solutions enhances data collection and facilitates remote monitoring and timely interventions, particularly in scenarios where in-person visits may be challenging (12).
Genetic and Personalized Medicine Approaches
Advancements in genetic research are paving the way for personalized medicine in migraine care. Understanding the genetic underpinnings of migraines can guide the development of targeted interventions tailored to an individual's unique genetic profile. This personalized approach could revolutionize treatment strategies, allowing for more precise and effective interventions based on the genetic factors contributing to a person's migraines (13).
Exploration of Lifestyle and Environmental Influences
Upcoming research increasingly focuses on the intricate interplay between lifestyle, environmental factors, and migraines; and studies examining the impact of factors such as diet, sleep patterns, and environmental triggers contribute valuable insights (13). For instance, research may reveal specific dietary components that act as triggers or protective factors for migraines, allowing healthcare professionals to offer targeted lifestyle recommendations.

Self Quiz
Ask yourself...
- What recent research findings have emerged regarding migraine prevention?
- How are digital health technologies and telemedicine being incorporated into upcoming research on migraine management?
- In personalized medicine, how is genetic research influencing upcoming approaches to migraine care?
- How can consideration of lifestyle factors and environmental influences contribute to a more holistic approach of migraine management?
Conclusion
In conclusion, this course focused on empowering learners not only with knowledge about migraine management, but with the practical insights and skills crucial for excellence in migraine care. The journey doesn’t end here; it extends into the realm of compassionate practice, where the combination of scientific understanding and safety measures transforms care providers into formidable advocates for those navigating the complexities of migraines.
Asthma Treatment and Monitoring
Introduction
When hearing the phrase asthma, what comes to mind? If you're an advanced practice registered nurse (APRN) with prescriptive authority, you've definitely heard of asthma before. Even as a nurse or maybe before nursing school, conversations about prescription drug use and respiratory health existed every so often.
Presently, patients seek guidance and information on various health topics from APRNs, including medication management and respiratory health. The information in this course will serve as a valuable resource for APRNs with prescriptive authority of all specialties, education levels, and backgrounds, to learn more about medications that can treat and manage asthma.
Defining Asthma
What Is Asthma?
Asthma is a non-communicable chronic health condition that affects the airways of the lungs and affects millions of people nationwide. Asthma is often diagnosed in childhood and can resolve in adulthood or continue for the rest of a patient's life. Several studies postulate the cause of asthma, but there is no definitive cause.
Genetics, age, environmental exposures, smoking, and a history of allergies are thought to play a role in asthma severity and development. Clinical presentation of asthma often includes trouble breathing, chronic airway inflammation, and airway hyperresponsiveness. Assessment for asthma often includes patient history, clinical presentation, spirometry testing, and pulmonary function tests (PFTs).
What Are the Stages of Asthma?
Since asthma is a chronic condition, several established guidelines can be used to determine the severity of asthma and explore possible medication options. Depending on the stage of asthma and patient response to existing therapy, treatment and management vary.
The four stages of asthma include intermittent, mild, moderate, and severe. Based on the 2020 National Asthma Education and Prevention Program (NAEPP) guidelines, here is the standard criteria for what constitutes each stage of asthma (2).
Intermittent asthma is characterized with the following clinical presentation and assessment (2):
- Patient history of respiratory symptoms, such as cough, trouble breathing, wheezing, or chest tightness <2 times a week
- Asthmatic flare-ups are short-lived with varying intensity
- Symptoms at night are <2 a month
- No asthmatic symptoms between flare-ups
- Lung function test FEV 1 at >80% above normal values
- Peak flow has <20% variability am-to-am or am-to-pm, day-to-day
Mild persistent asthma is characterized with the following clinical presentation and assessment (2):
- Patient history of respiratory symptoms, such as cough, trouble breathing, wheezing, or chest tightness 3-6 times a week
- Asthmatic flare-ups may affect activity level and can vary in intensity
- Symptoms at night are 3-4 times a month
- Lung function test FEV1 is >80% above normal values
- Peak flow has less than 20-30% variability
Moderate persistent asthma is characterized with the following clinical presentation and assessment (2):
- Patient history of respiratory symptoms, such as cough, trouble breathing, wheezing, or chest tightness daily
- Asthmatic flare-ups may affect activity level and can vary in intensity
- Symptoms at night are >5 times a month
- Lung function test FEV1 is 60%-80% of normal values
- Peak flow has more than 30% variability
Severe persistent asthma is characterized with the following clinical presentation and assessment (2):
- Patient history of respiratory symptoms, such as cough, trouble breathing, wheezing, or chest tightness continuously
- Asthmatic flare-ups affect activity level and often vary in intensity
- Asthmatic symptoms at night are constant
- Lung function test FEV1 is <60% of normal values
- Peak flow has more than 30% variability
Based on patient history, clinical presentation, and these criteria, treatment can be administered to decrease the symptoms of the patient. If a patient presents with symptoms that are outside of your scope of work or understanding, you can always refer patients to a pulmonologist or asthma specialist.
Often times, more severe cases of asthma and asthma emergencies require increased frequency and dosing of asthma-related medications. Health care provider professional discretion and patient condition should guide therapy. Consider reviewing a patient's medication history, pulmonary function, and health history prior to prescribing asthma medications (1).
What Are Asthmatic Emergencies?
Asthmatic emergencies are if a patient has asthma symptoms that are beyond what they typically experience and are unable to function without immediate medical intervention. Asthma emergencies can occur as a result of a patient being unable to access their asthmatic medications, being exposed to a possible allergen, or being under increased stress on the body.
Asthmatic emergencies often require collaborative medical intervention, increased dosages of medications discussed below, and patient education to prevent future asthmatic emergencies (1).
What If Asthma Is Left Untreated?
Depending on the clinical presentation and severity of asthma, asthma can cause several long-term complications if left untreated. If asthma is not properly managed, several complications, such as chronic obstructive pulmonary disease (COPD), decreased lung function, permanent changes to the lungs' airways, and death can occur (1, 2).
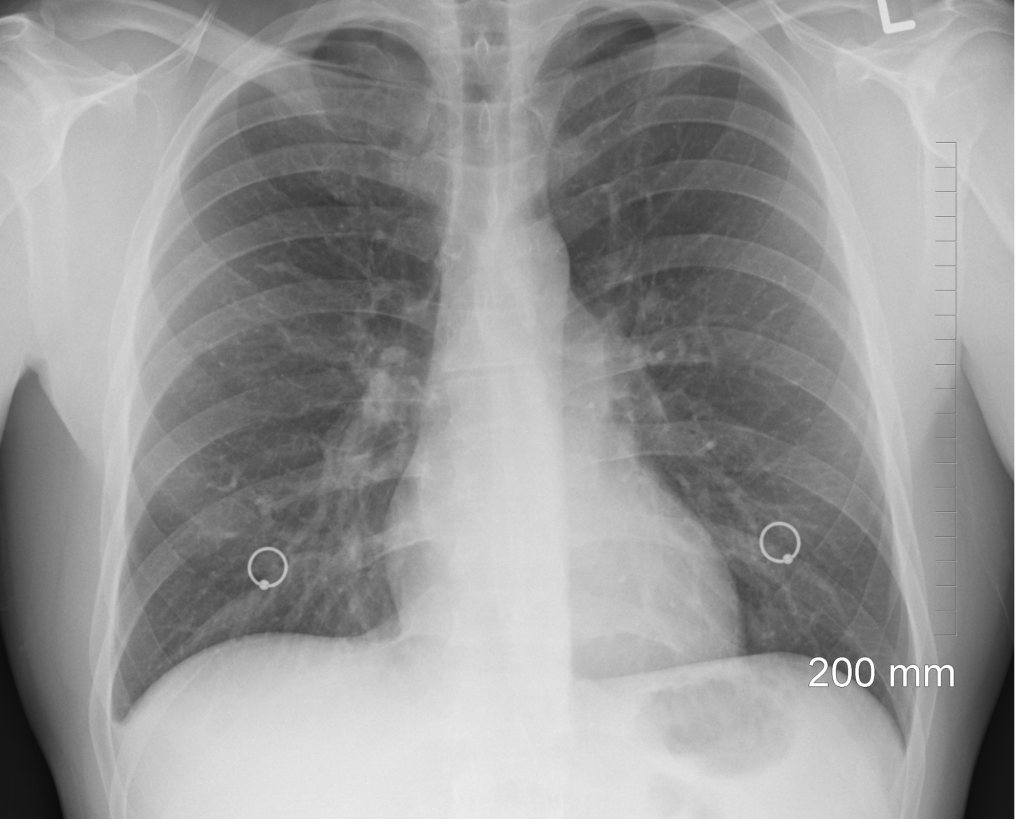
Defining Asthma Medications
What Are Commonly Used Medications to Manage Asthma?
Commonly used medications to manage asthma include inhaled corticosteroids, oral corticosteroids, short-acting beta agonists (SABAs), long-acting beta agonists (LABAs), long-acting muscarinic antagonists (LABAs), adenosine receptor antagonists, leukotriene modifiers, mast cell stabilizers, and monoclonal antibodies. The dosage, frequency, amount of asthma management medications, and medication administration route can all vary depending on clinical presentation, patient health history, and more.
How and Where are Asthma Medications Used?
Asthma medications can be used routinely or as needed for management of asthma symptoms depending on the patient. Asthma medications can be used at home, in public, and in health care facilities. Depending on the specific asthma medication and dosage, these medications can be taken by mouth, by an external device, such as an inhaler, via subcutaneous injection, or via intravenous solution (1).
What Are the Clinical Criteria for Prescribing Asthma Medication?
Clinical criteria for prescribing asthma medication can depend on the clinical presentation of a patient. Assessment of lung health and patient history are essential to determining the dosage and medications needed for adequate asthmatic symptom control.
Clinical guidelines from reputable organizations, such as the National Asthma Education and Prevention Program (NAEPP), the National Institutes of Health (NIH), the Global Initiative for Asthma (GINA), and the American Academy of Family Physicians (AAFP) can provide insight into the latest recommendations for asthma management (1, 2). In addition, local laws or health departments might have recommendations for asthma medication guidelines.
What Is the Average Cost for Asthma Medications?
Cost for asthma medications can significantly vary depending on the type of medication, insurance, dosage, frequency, medication administration route, and other factors. Cost is among a leading reason why many patients cannot maintain their medication regime (3). If cost is a concern for your patient, consider reaching out to your local pharmacies or patient care teams to find cost effective solutions for your patients.


Self Quiz
Ask yourself...
- What are some common signs of asthma?
- What are some common medications that can be prescribed to manage asthma?
- What are some factors that can influence asthma development and severity?
Inhaled Corticosteroids Pharmacokinetics
Health care provider professional discretion and patient condition should guide therapy. Consider reviewing a patient's medication history and health history prior to prescribing asthma medications.
Drug Class – Inhaled Corticosteroids
Commercially available inhaled corticosteroids include: ciclesonide (Alvesco HFA), fluticasone propionate (Flovent Diskus, Flovent HFA, Armon Digihaler), budesonide (Pulmicort Flexhaler), beclomethasone dipropionate (QVAR RediHaler), fluticasone furoate (Arnuity Ellipta), and mometasone furoate (Asmanex HFA, Asmanex Twisthaler).
Clinical criteria for prescribing an inhaled corticosteroid includes adherence to the latest clinical guidelines, patient medical history, patient clinical presentation, and drug availability (4).
Inhaled Corticosteroids Method of Action
Inhaled corticosteroids have an intricate mechanism of action involving several responses to the immune system. Inhaled corticosteroids decrease the existing initial inflammatory response by decreasing the creation and slowing the release of inflammatory mediators. Common inflammatory mediators include histamine, cytokines, eicosanoids, and leukotrienes. Inhaled corticosteroids can also induce vasoconstrictive mechanisms, which, as a result, can lead to less blood flow, resulting in less discomfort and edema (4).
In addition to anti-inflammatory properties, inhaled corticosteroids can create a localized immunosuppressive state that limits the airways' hypersensitivity reaction, which is thought to reduce bronchospasms and other asthma-associated symptoms. It is important to note that inhaled corticosteroids often do not produce therapeutic effects immediately, as many patients may not see a change in their asthma symptoms for at least a week after beginning inhaled corticosteroid therapy (4).
Inhaled Corticosteroids Side Effects
Every medication has the possibility of side effects, and inhaled corticosteroids are no exception. Common side effects of inhaled corticosteroids include oral candidiasis (thrush), throat irritation, headache, and cough.
Patient education about rinsing their mouth and oral hygiene after use is essential to avoid the possibility of thrush and other oral infections and irritations. More severe side effects can include prolonged immunosuppression, reduction in bone density, and adrenal dysfunction (4).
Inhaled Corticosteroids Alternatives
While there are clinical criteria for asthma medications, everyone can respond to medications differently. Some patients might not report their symptoms alleviating with inhaled corticosteroids, so additional medication, increased dosage, a change in frequency, or a new medication class might need to be considered (4).

Self Quiz
Ask yourself...
- What are some possible side effects of inhaled corticosteroids?
- What are some patient considerations to keep in mind when prescribing inhaled corticosteroids?
Oral Corticosteroids Pharmacokinetics
Health care provider professional discretion and patient condition should guide therapy. Consider reviewing a patient's medication history and health history prior to prescribing asthma medications.
Drug Class – Oral Corticosteroids
Commercially available oral corticosteroids include methylprednisolone, prednisolone, and prednisone. Clinical criteria for prescribing an oral corticosteroid includes adherence to the latest clinical guidelines, patient medical history, patient clinical presentation, and drug availability (4).
Oral Corticosteroids Method of Action
Methylprednisolone and prednisolone have a method of action as intermediate, long-lasting, synthetic glucocorticoids, have COX-2 inhibitory properties, and inhibit the creation of inflammatory cytokines (5).
Prednisone is a prodrug to prednisolone and has anti-inflammatory and immunomodulating glucocorticoid properties. Prednisone has a method of decreasing inflammation by reversing increased capillary permeability and suppressing the movement of certain leukocytes (6).
Oral Corticosteroids Side Effects
Every medication has the possibility of side effects, and oral corticosteroids are no exception. Methylprednisolone and prednisolone have possible side effects of skin changes, weight gain, increased intraocular pressure, neuropsychiatric events, neutrophilia, immunocompromised state, fluid retention, and GI upset.
Consider monitoring symptoms and overall health of patients on systemic corticosteroids to assess for long-term side effects (5). Prednisone has possible side effects of changes in blood glucose, changes in sleep habits, changes in appetite, increased bone loss, an immunocompromised state, changes in adrenal function, and changes in blood pressure (6).
Oral Corticosteroids Alternatives
While there are clinical criteria for asthma medications, everyone can respond to medications differently. Some patients might not report their symptoms alleviating with oral corticosteroids, so additional medication, increased dosage, a change in frequency, or a new medication class might need to be considered (6).

Self Quiz
Ask yourself...
- What are some possible side effects of oral corticosteroids?
- What are some patient considerations to keep in mind when prescribing oral corticosteroids versus inhaled corticosteroids?
Short-Acting Beta Agonists (SABAs)
Health care provider professional discretion and patient condition should guide therapy. Consider reviewing a patient's medication history and health history prior to prescribing asthma medications.
Drug Class – SABAs
Common commercially available SABAs include albuterol sulfate (ProAir HFA, Proventil HFA, Ventolin HFA), albuterol sulfate inhalation powder (ProAir RespiClick, ProAir Digihaler), levalbuterol tartrate (Xopenex HFA), and levalbuterol hydrochloride (Xopenex) (4).
SABAs Method of Action
Short-acting beta-agonists (SABAs) have a rapid onset as broncho-dilating medications. SABAs, especially albuterol in emergent situations, are used often to quickly relax bronchial smooth muscle from the trachea to the bronchioles through action on the β2-receptors.
While SABAs are effective bronchodilators in the short term for asthma symptoms, SABAs do not affect the underlying mechanism of inflammation. As a result, SABAs are often used for short-acting intervals, such as few hours, and have limited capabilities to prevent asthma exacerbations alone (4). SABAs can be administered via meter-dosed inhalers, intravenous, dry powder inhalers, orally, subcutaneously, or via nebulizer.
SABAs Side Effects
Every medication has the possibility of side effects, and SABAs are no exception. Because of the beta receptor agonisms, possible SABA side effects include increased heart rate, chest pain, chest palpitations, body tremors, and nervousness (4). Because of the short half-life of SABAs, chronic side effects are not typically observed.
SABAs Alternatives
While there are clinical criteria for asthma medications, everyone can respond to medications differently. Some patients might not report their symptoms alleviating with SABAs, so additional medication, increased dosage, a change in frequency, or an additional medication class might need to be considered (4).

Self Quiz
Ask yourself...
- What are some possible side effects of short-acting beta agonists?
- What are some patient considerations to keep in mind when prescribing SABAs?
Long-Acting Beta Agonists (LABAs)
Health care provider professional discretion and patient condition should guide therapy. Consider reviewing a patient's medication history and health history prior to prescribing asthma medications.
Drug Class – LABAs
Common commercially available LABAs are salmeterol and formoterol (7).
LABAs Method of Action
Long-acting beta-agonists (LABAs) have a rapid onset like SABAs, but also have a longer half-life. LABAs are used often as asthma maintenance medications to relax bronchial smooth muscle from the trachea to the bronchioles through action on the β2-receptors. While SABAs are effective bronchodilators in the short term for asthma symptoms, LABAs are effective bronchodilators in the long term for asthma symptoms.
Like SABAs, LABAs do not affect the underlying mechanism of inflammation. LABAs can be administered via meter-dosed inhalers, intravenous, dry powder inhalers, orally, subcutaneously, or via nebulizer. LABAs are often effective for 12-hour durations (7).
LABAs Side Effects
Every medication has the possibility of side effects, and LABAs are no exception. Like SABAs, because of the beta receptor agonisms, possible LABA side effects include increased heart rate, chest pain, chest palpitations, body tremors, and nervousness (7). Other more prolonged side effects can include changes in blood glucose levels and changes in potassium levels with prolonged LABA use (7).
LABAs Alternatives
While there are clinical criteria for asthma medications, everyone can respond to medications differently. Some patients might not report their symptoms alleviating with LABAs, so additional medication, increased dosage, a change in frequency, or an additional medication class might need to be considered (4).
In addition, there are combination inhaled corticosteroid/LABA medications that can be considered, such as fluticasone propionate and salmeterol (Advair Diskus, Advair HFA, AirDuo Digihaler, AirDuo RespiClick, Wixela Inhub), fluticasone furoate and vilanterol (Breo Ellipta), mometasone furoate and formoterol fumarate dihydrate (Dulera), and budesonide and formoterol fumarate dihydrate (Symbicort) (4).

Self Quiz
Ask yourself...
- What are some possible side effects of LABAs?
- What are some patient considerations to keep in mind when prescribing SABAs compared to LABAs?
Long-Acting Muscarinic Antagonists (LAMAs)
Health care provider professional discretion and patient condition should guide therapy. Consider reviewing a patient's medication history and health history prior to prescribing asthma medications.
Drug Class – LAMAs
Common commercially available LAMAs include two inhalation powders via inhalers known as tiotropium bromide (Spiriva Respimat) and fluticasone furoate, umeclidinium, and vilanterol (Trelegy Ellipta) (4).
LAMAs Method of Action
Both drugs mentioned above are long-acting muscarinic antagonists (LAMAs). LAMAs work to alleviate asthmatic symptoms by antagonizing the type 3 muscarinic receptors in bronchial smooth muscles, resulting in relaxation of muscles in the airway (4). Because LAMAs are long-acting, they are not recommended for cases of acute asthma exacerbations or asthmatic emergencies (4).
LAMAs Side Effects
Possible LAMA side effects include urinary retention, dry mouth, constipation, and glaucoma (4).
LAMAs Alternatives
While there are clinical criteria for asthma medications, everyone can respond to medications differently. Some patients might not report their symptoms alleviating with LAMAs, so additional medication, increased dosage, a change in frequency, or an additional medication class might need to be considered (4).

Self Quiz
Ask yourself...
- What are some possible side effects of LAMAs?
- What are some patient considerations to keep in mind when prescribing LAMAs?
Adenosine Receptor Antagonists Pharmacokinetics
Health care provider professional discretion and patient condition should guide therapy. Consider reviewing a patient's medication history and health history prior to prescribing asthma medications.
Drug Class – Adenosine Receptor Antagonists
The commercially available adenosine receptor antagonist for asthma management is theophylline as a pill or intravenous (8).
Adenosine Receptor Antagonists Method of Action
The method of action for theophylline is acting as a nonselective adenosine receptor antagonist, acting as a competitive, nonselective phosphodiesterase inhibitor, and reducing airway responsiveness to histamine, allergens, and methacholine (8).
Adenosine Receptor Antagonists Side Effects
Common side effects of theophylline include GI upset, headache, dizziness, irritability, and arrythmias (8).
Adenosine Receptor Antagonists Alternatives
While there are clinical criteria for asthma medications, everyone can respond to medications differently. Some patients might not report their symptoms alleviating with theophylline, so additional medication, increased dosage, a change in frequency, or an additional medication class might need to be considered (4).

Self Quiz
Ask yourself...
- What are some possible side effects of adenosine receptor antagonists?
- What are some patient considerations to keep in mind when prescribing adenosine receptor antagonists?

Leukotriene Modifiers Pharmacokinetics
Health care provider professional discretion and patient condition should guide therapy. Consider reviewing a patient's medication history and health history prior to prescribing asthma medications.
Drug Class – Leukotriene Modifiers
Commercially available leukotriene modifiers include montelukast (Singular) and zafirlukast (Accolate) as oral pills taken once a day. Zileuton (Zyflo CR) is a 5-lipoxygenase inhibitor that also modifies leukotriene activity (4).
Leukotriene Modifiers Method of Action
Montelukast and zafirlukast work to control asthma-related symptoms by targeting leukotrienes, which are eicosanoid inflammatory markers. Montelukast works in particular by blocking leukotriene D4 receptors in the lungs, thus allowing decreased inflammation in the lungs and increased relaxation of lung smooth muscle (9).
Zafirlukast works by being a competitive antagonist at the cysteinyl leukotriene-1 receptor (CYSLTR1) (10). Zileuton is a 5-lipoxygenase inhibitor, in which 5-lipoxygenase is needed for leukotriene creation. Blocking 5-lipoxygenase decreases the formation of leukotrienes at several receptors. As a result of decreased leukotriene production, there is decreased inflammation, decreased mucus secretion, decreased bronchoconstriction (11).
Leukotriene Modifiers Side Effects
Possible side effects of montelukast include headaches, GI upset, and upset. Neuropsychiatric events, such as nightmares, changes in sleep, depression, and suicidal ideation are more severe side effects associated with montelukast.
Possible side effects of zafirlukast include headache, GI upset, and hepatic dysfunction (9).
Possible side effects of zileuton include hepatic dysfunction, changes in sleep, changes in mood, headaches, and GI upset. When the leukotriene modifiers, neuropsychiatric side effects are to be monitored for in particular, especially for suicidal ideation (9,10,11).
Leukotriene Modifiers Alternatives
Some patients might not report their symptoms alleviating with leukotriene modifiers, so additional medication, increased dosage, a change in frequency, or an additional medication class might need to be considered (4).

Self Quiz
Ask yourself...
- What are some possible side effects of leukotriene modifiers?
- What are some patient considerations to keep in mind when prescribing leukotriene modifiers?
Mast Cell Stabilizer Pharmacokinetics
Health care provider professional discretion and patient condition should guide therapy. Consider reviewing a patient's medication history and health history prior to prescribing asthma medications.
Drug Class – Mast Cell Stabilizer
A commercially available mast cell stabilizer is cromolyn available via metered-dose inhaler and nebulizer solution (12).
Mast Cell Stabilizer Method of Action
Cromolyn has a method of action in which it inhibits the release of inflammatory mediators from cells, such as the release of histamine and leukotrienes (12).
Mast Cell Stabilizer Side Effects
Every medication has the possibility of side effects, and cromolyn is no exception. Common side effects of cromolyn include dry throat, throat irritation, drowsiness, dizziness, cough, headache, and GI upset (12).
Mast Cell Stabilizer Alternatives
While there are clinical criteria for asthma medications, everyone can respond to medications differently. Some patients might not report their symptoms alleviating with mast cell stabilizers, so additional medication, increased dosage, a change in frequency, or an additional medication class might need to be considered (4).

Self Quiz
Ask yourself...
- What are some possible side effects of mast cell stabilizers?
- What are some patient considerations to keep in mind when prescribing mast cell stabilizers?
Monoclonal Antibody Pharmacokinetics
Health care provider professional discretion and patient condition should guide therapy. Consider reviewing a patient's medication history and health history prior to prescribing asthma medications.
Drug Class – Monoclonal Antibody
Commercially available monoclonal antibodies include Omalizumab (Xolair), mepolizumab (Nucala), reslizumab (Cinqair), benralizumab (Fasenra), dupilumab (Dupixent), and tezepelumab-ekko (Tezspire). Omalizumab, mepolizumab, benralizumab, dupilumab, and texepelumab-ekko are available via subcutaneous injection. Reslizumab is available via intravenous solution (4).
Monoclonal Antibody Method of Action
Omalizumab is an anti-IgE monoclonal antibody that works by inhibiting the binding of IgE to mast cells and basophils. As a result of decreased bound IgE, activation and release of mediators, such as histamine, in the allergic response are decreased (13).
Mepolizumab, reslizumab, and benralizumab are interleukin (IL)-5 antagonists. These IL-5 antagonists inhibit IL-5 signaling, allowing for a decrease in the creation and survival of eosinophils. However, the full method of action for IL-5 antagonists is still unknown, as more evidence-based research is needed (4, 15).
Dupilumab is an IgG4 antibody that inhibits IL-4 and IL-13 signaling by binding to the IL-4Rα subunit. This inhibition of the IL-4Rα subunit allows for the decrease of IL-4 and IL-13 cytokine-induced inflammatory responses (14).
Tezepelumab-ekko is an IgG antibody that binds to the thymic stromal lymphopoietin (TSLP) and prevents TSLP from interacting with the TSLP receptor. Blocking TSLP decreases biomarkers and cytokines associated with inflammation. Knowing this, the full method of action for Tezepelumab-ekko is still unknown, as more evidence-based research is needed4,15.
Monoclonal Antibody Side Effects
Possible side effects of omalizumab include injection site reactions, fracture, anaphylaxis, headache, and sore throat (13). Possible side effects of mepolizumab, reslizumab, and benralizumab include injection site reactions, headache, and hypersensitivity reactions (4). Possible side effects of dupilumab include joint aches, injection site reactions, and headache (14). Possible side effects of tezepelumab-ekko include injection site reactions and headache (14).
Monoclonal Antibody Alternatives
While there are clinical criteria for asthma medications, everyone can respond to medications differently. Some patients might not report their symptoms alleviating with monoclonal antibodies, so additional medication, increased dosage, a change in frequency, or an additional medication class might need to be considered (4).

Self Quiz
Ask yourself...
- What are some possible side effects of monoclonal antibodies?
- What are some patient considerations to keep in mind when prescribing monoclonal antibodies?
Nursing Considerations
Nurses remain the most trusted profession for a reason, and APRNs are often pillars of patient care in several health care settings. Patients turn to nurses for guidance, education, and support. While there is no specific guideline for the nurses' role in asthma education and management, here are some suggestions to provide quality care for patients currently taking medications to manage asthma or concerned about possibly having asthma.
- Take a detailed health history. Often times, respiratory symptoms, such as a cough or trouble breathing, are often dismissed in health care settings, or seen as "common symptoms with everyone." If a patient is complaining of symptoms that could be related to asthma, inquire more about that complaint.
Ask about how long the symptoms have lasted, what treatments have been tried, if these symptoms interfere with their quality of life, and if anything alleviates any of these symptoms. If you feel like a patient's complaint is not being taken seriously by other health care professionals, advocate for that patient to the best of your abilities.
- Review medication history at every encounter. Often times, in busy clinical settings, reviewing health records can be overwhelming. Millions of people take asthma medications at varying dosages, frequencies, and times of day. Many people with asthma take more than one medication to manage their symptoms.
Ask patients how they are feeling on the medication, if their symptoms are improving, and if there are any changes to medication history.
- Be willing to answer questions about asthma, respiratory health, and medication options. Society stigmatizes open discussions of prescription medication and can minimize symptoms of asthma, such as a chronic cough.
There are many people who do not know about medication options or the long-term effects of undiagnosed or poorly managed asthma. Be willing to be honest with yourself about your comfort level discussing topics and providing education on asthma medications and asthma clinical assessment options.
- Inquire about a patient's life outside of medications, such as their occupation, living situation, and smoking habits. Household exposures, such as carpets or pets, can trigger asthma. Occupations with high exposure to smoke can also trigger asthmatic symptoms. Smoking, living with someone who smokes, or residing in an area with high levels of pollution can also influence asthma symptoms.
Discuss possible solutions to help with symptoms, such as improving ventilation, increasing air quality, and mask wearing when possible.
- Communicate the care plan to other staff involved for continuity of care. For several patients, especially for patients with severe asthma, care often involves a team of nurses, specialists, pharmacies, and more. Ensure that patients' records are up to date for ease in record sharing and continuity of care.
- Stay up to date on continuing education related to asthma medications, as evidence-based information is always evolving and changing. You can then present your new learnings and findings to other health care professionals and educate your patients with the latest information. You can learn more about the latest research on asthma and asthma-related medications by following updates from evidence-based organizations.
How can nurses identify if someone has asthma?
Unfortunately, it is not always possible to look at someone with the naked eye and determine if they have asthma. While some people might have visible asthmatic symptoms, such as wheezing or trouble breathing, asthmatic clinical presentation can significantly vary from person to person.
APRNs can identify and diagnose if someone has asthma by taking a complete health history, listening to patient's concerns, and offering pulmonary function testing.
What should patients know about asthma medications?
Patients should know that anyone has the possibility of experiencing side effects medications for asthma management, just like any other medication. Patients should be aware that if they notice any changes in their mood, experience any sharp headaches, or feel like something is a concern, they should seek medical care.
Nurses should also teach patients to advocate for their own health in order to avoid untreated or undetected asthma and possible chronic complications from asthma or asthma-related medications.
Here are important tips for patient education in the inpatient or outpatient setting:
- Tell the health care provider of any existing medical conditions or concerns (need to identify risk factors).
- Tell the health care provider of any existing lifestyle concerns, such as tobacco use, other drug use, sleeping habits, occupation, diet, menstrual cycle changes (need to identify lifestyle factors that can influence asthmatic medication use, asthma severity, and asthma management).
- Tell the health care provider if you have any changes in your breathing, such as pain with deep breathing or persistent coughing (potential asthma exacerbation symptoms or possibility of asthma medications not being as effective for treatment).
- Tell the nurse of health care provider if you experience any pain that increasingly becomes more severe or interferes with your quality of life.
- Keep track of your health, medication use, and health concerns via an app, diary, or journal (self-monitoring for any changes).
- Tell the health care provider right away if you are having thoughts of hurting yourself or others (possible increased risk of suicidality is a possible side effect for montelukast use).
- Take all prescribed medications as indicated and ask questions about medications and possible other treatment options, such as non-pharmacological options or surgeries.
- Tell the health care provider if you notice any changes while taking medications or on other treatments to manage asthma (potential worsening or improving health situation).

Self Quiz
Ask yourself...
- What are some problems that can occur if medications are not asthma properly?
- What are some possible ways you can obtain a detailed, patient centric health history?
- What are some possible ways APRNs can educate patients on asthma and air quality?
Research Findings
What Research on Asthma Medication Exists Presently?
There is extensive publicly available literature on asthma and asthma-related medications via the National Institutes of Health and other evidence-based journals (1,2,4).
What are some ways for people who take asthma medications to become a part of research?
If a patient is interested in participating in clinical trial research, they can seek more information on clinical trials from local universities and health care organizations.

Self Quiz
Ask yourself...
- What are some reasons someone would want to enroll in clinical trials?
Conclusion
Asthma is a chronic condition that affects many people from their childhood to their aging years. As more medications for asthma come onto the market and more evidence-based approaches to asthma and lung care emerge, APRNs will be at the forefront of primary care and asthma care across the lifespan.
Case Study #1
Susie is a mom to a 15-year-old named Jill. She arrives at the pediatric asthma and allergy specialist practice for a new patient visit. Susie reports that she notices Jill is having trouble sleeping at night and coughing more during the day for the past month. Jill plays soccer with her school, but her mom is concerned about coughing and trouble sleeping interfering with her sports.
Susie knows that her dad has asthma, and Jill spends a lot of time with her aunt who smokes cigarettes. Jill has a history of generalized anxiety disorder and reports no smoking, no drinking, and no recreational drugs. Jill also wants to learn more about her lung health, as she wants to play soccer professionally one day.
- What are some specific questions you’d want to ask about Jill’s coughing and respiratory health?
- What are health history questions you would want to highlight?
- What are some tests or lab work would you suggest performing?

Case Study #2 (Continued)
Susie also shares that she is dating a new partner who vapes in the home, and they recently got a pet puppy in the home. She states that Jill had trouble sleeping at night and coughing a lot when she was younger, but Susie thought Jill grew out of it. Susie wants to learn more about if Jill has asthma like her grandfather, if there are any ways to manage this cough, and if there are any tests that can determine Jill’s lung health in the office today.
- What sort of tests can be done in-office to assess pulmonary function?
- What sort of environmental exposures can trigger respiratory conditions?
Susie agrees to have Jill do allergy testing and to do an in-office pulmonary function test for teenagers. Jill also wants to learn more about spirometry that you mentioned earlier and how to monitor her health outside of the office since she’s busy with school and soccer and doesn’t want to come to the office every time there’s a problem.
Susie is open to medication options for Jill but doesn’t want anything that will interfere too much with Jill’s social time with her friends. Susie and Jill also want to know if this is a health condition that Jill will have forever or if Jill will grow out of this.
- Knowing Susie’s concerns and Jill’s age, what are some talking points about reducing possible asthma triggers?
- How would you explain asthma as a chronic health condition to an adolescent patient?
- Given Jill and Susie’s concerns about medications, what would be some possible medication options to consider after reviewing Jill’s pulmonary function test results and patient history?
References + Disclaimer
- Abi-Aad, K., & Derain, A. (2023, August 17). Hydromorphone. Retrieved from Stat Pearls: https://www.ncbi.nlm.nih.gov/books/NBK470393/
- Adler, J., Ballantyne, J., Chou, R., Davies, P., Fanciullo, G., & Fine, P. (2009). Clinical Guidelines for the Use of Chronic Opioid Therapy in Chronic NonCancer Pain. The Journal of Pain, 113-130.
- Ahmad, F., Rossen, L., Sutton, P., & & Talih, M. (2018). Provisional drug overdose. National Vital Statistics Reports, pp. 1-12.
- Altman, R., Clark, M., Huddart, R., & Klein, T. (2018, October 28). Pharm GKB Summary: Oxycodone Pathway, Pharmacokinetics. Retrieved from Pharmacogenet Genomics: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6602093/#:~:text=Approximately%2072%25%20of%20an%20oxycodone,oxycodone%20is%20unconjugated%20%5B70%5D
- Atrux-Tallau, N., naimi, Z., & Jaudinot, E. (2022, November 4). Pharmocokinetics of Morphine Sulfate Orodispersible tablets and Bioequivalence with Immediate-Release Oral Morphine Sulfate Formulations in Healthy Adult SubjectsUnder fastin Conditions. Retrieved from Clinical Drig Investigation: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9705466/
- Baldwin, G., Compton, W. M., Han, B., Houry, D., Jones, C. M., & Vivolo-Kantor, A. (2021, September 24). Methamphetamine use in the United States: epidemiological update and implocations for prevention, treatment and harm reduction. Annual New York Academy of Science. New York: National Institute of Health.
- Berg, K. A., & Clarke, W. P. (2018). Making Sense of Pharmacology: Inverse Agonism and Functional Selectivtiy. International Journal of Neuropsychopharmacology, 962-977.
- Bistas, K., Lopez-Ojeda, W., & Ramos-Matos, C. (2023, May 29). Fentanyl. Retrieved from Stat Pearls: https://www.ncbi.nlm.nih.gov/books/NBK459275/
- Blyth, F., Briggs, A., Hoy, D. G., March, L. M., & Schneider, C. H. (2019). The Global Burden of Musculoskeletal Pain-Where to From Here? American Journal of Public Health, 35-40.
- Bramanti, P., Cavalli, E., Mammana, S., Mazzon, E., & Nicoletti, F. (2019). The neuropathic pain: An Overview of the current treatment and future therapeutic approaches. International Journal of Immunopathology and Pharmacology, 33.
- Brennan, F., Carr, D., Cousins, M., & Pain, D. (2013). Pain Management: A Fundamental Human Right. Anesthesia and Analgesia, 224-227.
- Carver, A. C., & Foley, K. (2003). Types of Pain. In D. Kufke, & R. W. Pollock, Cancer Medicine. Hamilton: Holland Frei Cancer Medicine.
- Centers for Disease Control and Prevention. (2022). CDCs Clinical Practice Guidelines for Prescribing Opioids. Retrieved from Opioids: https://www.cdc.gov/opioids/healthcare-professionals/prescribing/guideline/index.html?s_cid=DOP_Clinician_Search_Paid_001&gclid=CjwKCAjwrranBhAEEiwAzbhNtVKOCMzLLnwhfj7B2D_aBCZM_SryNcEyXl0GRigmorFhKve2ekCVrhoCNYQQAvD_BwE
- Centers for Disease Control and Prevention. (2023, August 8). Opioids. Retrieved from Centers for Disease Control and Prevention: https://www.cdc.gov/opioids/basics/epidemic.html#print
- Chiang, N., Gyaw, S., & Krieter, P. A. (2019). Comparison of the Pharmacokinetic Properties of Naloxone Following the Use of FDA-Approved Intranasal and Intramuscular Devices Versus a Common Improvised Nasal Naloxone Device. Journal of Clinical Pharmacology, 1078-1084.
- Cicero, T., & Ellis, M. &. (2017). The changing face of heroin use in the United States: A retrospective analysis of the past 50 years. JAMA, 673-681.
- Cofano, S., & Yellon, R. (2022, October 24). Stat Pearls: Hydrocodone. Retrieved from National Institutes of Health: https://www.ncbi.nlm.nih.gov/books/NBK537288/
- Dart, R., Hoyte, C., & Nakhee, S. (2021). A Review on Tramadol Toxicity: Mechanism of Action, Clinical Presentation, and Treatment. Forensic Toxicology, 293-310. Retrieved from Forensic Toxicology: https://link.springer.com/article/10.1007/s11419-020-00569-0
- Delsignor, R. e. (2001). Lofexidine versus clonidine in rapid opiate detoxification. Journal of Substance Abuse Treatment, 11-17.
- Department of Defense Veterans Association. (2023). Defense and Veterans Pain Rating Scale. Retrieved from VA.gov: https://www.va.gov/PAINMANAGEMENT/docs/DVPRS_2slides_and_references.pdf
- Department of Health and Aged Care. (2013, January 20). FLACC Pain Scale. Retrieved from health.gov: https://www1.health.gov.au/internet/publications/publishing.nsf/Content/triageqrg~triageqrg-pain~triageqrg-FLACC
- Donaldson, S. L. (2017). Provider-Based Interventions to Mitigate Risk for Opioid Pain Medication Abuse Among Adult Patients in a Primary Care Setting.
- Dydyk, A. M., & Grandhe, S. (2023, January 29). Pain Assessment. Retrieved from STAT PEARLS: https://www.ncbi.nlm.nih.gov/books/NBK556098/#:~:text=Pain%20is%20the%20most%20common,pain%20in%20the%20United%20States.
- Fan, M., Hamilton, M., Hyland, B., & Tscheng, D. (2019). Diversion of Controlled Drugs in Hospitals: A Scoping review of Contributors and Safeguards. Journal of Hospital Medicine.
- GeriatricPain.org. (2022, January). Fast Facts: Selected Pain Assessment Tools. Retrieved from Geriatricpain.org: Geriatricpain.org https://geriatricpain.org/selected-pain-assessment-tools-fc
- Haffajee, R., Jena, A., Weiner, S., & & Kesselheim, A. (2019). Mandatory use of prescription drug monitoring programs. Journal of the American Medical Association, 1667-1668.
- International Association for the Study of Pain . (2020, July 16). IASP Announces Revised Definition of Pain. Retrieved from International Association for the Study of Pain: https://www.iasp-pain.org/publications/iasp-news/iasp-announces-revised-definition-of-pain/
- JAMA. (2023). Substance Use and Addiction Medicine. Retrieved from JAMA Network: https://jamanetwork.com/collections/5921/substance-use-and-addiction-medicine
- John, W. S., Schwartz, R. P., Subramanian, G., & Wu, L.-T. (2018). Prevalence, Patterns and correlates of multiple substance use disorders among adults. Drug and Alcohol Dependency, 79-87.
- Jones, C., Einstein, E., & Compton, W. (2018). Changes in synthetic opioid involvement in drug overdose deaths in the United States. JAMA, 1819-1821.
- Kalava, A., King, K. C., & Preuss, C. V. (2023, April 29). Perscription of Controlled Substances: Benefits and Risks. Retrieved from STAT PEARLS: https://www.ncbi.nlm.nih.gov/books/NBK537318/
- Khalid, N., Patel, P., & Singh, A. (2023, January). Cannabis Versus Opioids for Pain. Retrieved from Stat Pearls: https://www.ncbi.nlm.nih.gov/books/NBK573080/
- Kreutzwiser, D., & Tawfic, Q. (2020). Mathadone for Pain Management. A Pharmacotherapeutic Review, 827-839.
- Kroenke, K., Spiter, R., Williams, J., & Lowe, B. (2011, Nov). An ultra-brief screening scale for anxiety and depression: the PHQ-4. From Principles of Neuropathic Pain Assessment and Management, 613-21. Psychosomatics 2009.
- Manchikanti, L., Kaye, A., Knezevic, N., McAnally, H., Slavin, K., Trescot, A., & Hirsch, J. (2018). Responsible, safe, and effective prescription of opioids for chronic non-cancer pain: American Society of Interventional Pain Physicians guidelines. Pain Physician, S3-S92.
- Marquez, C. B. (2020). Changing the outlook toward the problem of opioid addiction: From “War on Drug” to “Public Health Emergency”. Seton Hall: Law Student Scholarship.
- Marsch, L., Borodovsky, J., & Dallery, J. (2019). Advances in the psychosocial treatment of addiction: The role of technology in the delivery of evidence-based psychosocial treatment. The Psyciatric Clinics of North America, 585-596.
- McLellan, T., & Volkow, N. (2016). Opioid Abuse in Chronic Pain-Misconceptions and Mitigation Strategies. New England Journal of Medicine, 1253-1263.
- National Institute of Drug Abuse (NIDA). (2023, August 30). Prescription Opioid Drug Facts. Retrieved from National Institute on Drug Abuse: https://nida.nih.gov/publications/drugfacts/prescription-opioids
- National Institute of Health. (2023, August 25). Medications for Opioid Overdose, Withdrawal, & Addiction. Retrieved from National Institute of Drug Addiction: https://nida.nih.gov/research-topics/opioids/medications-opioid-overdose-withdrawal-addiction-infographic
- Pain Physician. (2008). Opioid Special Issue. Pain Physician, S133-S153.
- Ransford, e. a. (2019, February 08). The Ransford Pain Drawing . Retrieved from compassionandsupport.org: https://compassionandsupport.org/wp-content/uploads/sites/2/2019/08/PainScaleRansford.pdf
- Rudd, R. A., Zibbell, J., & Gladden, M. (2016). Increases in drug and opioid overdose deaths-Untied States. Morbidity and Mortlity Weekly Report, 1378-1382.
- SAMHSA. (2020). Key Substance Use and Mental Health Indicators in the United States: Ressults from the 2019 National Survey on Drug Use and Health. SAMHSA.
- Scalpel, S. (2016, November). The Joint Commission Deserves Some Blame for the Opioid Crisis. Retrieved from Missouri Medicine: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6139759/
- Scholl, L., Seth, P., Kariisa, M., Wilson, N., & Baldwin, G. (2019). Drug and opioid-involved overdose deaths-Unioted States, 2013-2017. Morbidity and Mortatlity Weekly Report 67, 1419-1427.
- Stauffer, L., & Gibson, S. (2017). The Nurse’s Role in Identifying and Educating Patients At Risk for Opioid Abuse. AAACN Viewpoint, 1.
- The Joint Commission. (2023, January). The Joint Commission History Timeline. Retrieved from JointCommission.org: https://www.jointcommission.org/-/media/tjc/documents/tjc-history-timeline-through-2022.pdf
- Toombs, K., Kral, L., Colleran, C., & & Varney, S. (2018). Nurse practitioner-pharmacist collaboration in pain management: Strategies for success. . Journal of the American Association of Nurse Practitioners, 141-148.
- U.S. Food and Drug Administration. (2023, May 23). FDA. Retrieved from Information about Medication Assisted Treatment (MAT): https://www.fda.gov/drugs/information-drug-class/information-about-medication-assisted-treatment-mat
- Volkow, N., Jones, E., Einstein, E., & Wargo, E. (2019). Prevention and Treatment of Opioid mIsuse and Addiction: A Review. JAMA Psychiatry, 208-216.
- Katie Kerwin McCrimmon, Uch. (2023, May 15). What is Mounjaro? and does it work better for weight loss than Ozempic and Wegovy?. UCHealth Today. https://www.uchealth.org/today/what-is-mounjaro-and-how-does-it-work-for-weight-loss/
- National Institutes of Health. (2023, July 28). DailyMed – mounjaro- tirzepatide injection, solution. U.S. National Library of Medicine. https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=d2d7da5d-ad07-4228-955f-cf7e355c8cc0
- Type 2 Diabetes Treatment to Lower A1C | Mounjaro® (tirzepatide). (2023). https://www.mounjaro.com/?utm_id=go_cmp-16966473997_adg-133042365262_ad-626584063672_kwd-1651326559888_dev-c_ext-_prd-_mca-_sig-EAIaIQobChMIxcXZqYeHgQMVhDjUAR2Lvw5CEAAYASAAEgIMkfD_BwE&utm_source=google&utm_medium=ppc&campaign=16966473997&adgroup=133042365262&ad=626584063672&utm_keyword=kwd-1651326559888&gclid=EAIaIQobChMIxcXZqYeHgQMVhDjUAR2Lvw5CEAAYASAAEgIMkfD_BwE
- GoodRX – error. (2023, July 14). https://www.goodrx.com/mounjaro/how-make-you-feel
- Chen, S. (2023, July 28). Diabetes drug Mounjaro shown to have extraordinary weight loss for people without diabetes. diaTribe. https://diatribe.org/diabetes-drug-mounjaro-shown-have-extraordinary-weight-loss-people-without-diabetes
- VA Pharmacy Benefits Management Services. (2022, August). Tirzepatide Injection Criteria for Use. https://www.va.gov/formularyadvisor/DOC_PDF/CFU_Tirzepatide_MOUNJARO_Criteria_Aug_2022.pdf.
- Allied PR. (2023 B.C.E., May 6). Mounjaro Weight Loss: Newly Launch Over The Counter Alternative Pills To Tirzepatide & Mounjaro Weight Loss. https://newsdirect.com/news/mounjaro-weight-loss-newly-launch-over-the-counter-alternative-pills-to-tirzepatide-and-mounjaro-weight-loss-300908569. Retrieved August 30, 2023, from https://newsdirect.com/news/mounjaro-weight-loss-newly-launch-over-the-counter-alternative-pills-to-tirzepatide-and-mounjaro-weight-loss-300908569
- Mounjaro (2023). Savings and support for Mounjaro. Retrieved on August 31st 2023 from https://www.mounjaro.com/savings-resources?gclid=Cj0KCQjw9MCnBhCYARIsAB1WQVWAcINPKFwiHl4SbZQiGC8E_o9wHVOkDJDDUuphW3OlsKBagVTF1rQaApLJEALw_wcB
- Global diabetes cases to soar from 529 million to 1.3 billion by 2050. (n.d.). The Institute for Health Metrics and Evaluation. https://www.healthdata.org/news-events/newsroom/news-releases/global-diabetes-cases-soar-529-million-13-billion-2050.
- Diabetes Research Institute Foundation. (2023, March 31). Diabetes Statistics – DRIF. DRIF. https://diabetesresearch.org/diabetes-statistics/#:~:text=37.3%20million%20people%2C%20or%2011.3,yet%20been%20diagnosed%20(2022)
- Manage blood sugar. (2021, April 28). Centers for Disease Control and Prevention. https://www.cdc.gov/diabetes/managing/manage-blood-sugar.html
- About the National Diabetes Prevention Program | CDC. (n.d.). https://www.cdc.gov/diabetes/prevention/about.htm#:~:text=The%20National%20Diabetes%20Prevention%20Program%E2%80%94or%20National%20DPP%E2%80%94was%20created,diabetes%20in%20
- Ms, M. G. R. (2023, February 16). All about Ozempic. Healthline. https://www.healthline.com/health/drugs/ozempic#_noHeaderPrefixedContent
- Professional, C. C. M. (n.d.). Ghrelin. Cleveland Clinic. https://my.clevelandclinic.org/health/body/22804-ghrelin#:~:text=Ghrelin%20and%20leptin%20are%20two,brain%20when%20you’re%20hungry
- Prelipcean, M., MD. (2020, June 22). Behind the counter: Glucagon-like peptide-1 receptor agonists for type 2 diabetes. https://www.medicalnewstoday.com/articles/glp-1-receptor-agonists-type-2-diabetes
- Mba, A. B. P. (2023, May 1). Ozempic side effects: What you should know. https://www.medicalnewstoday.com/articles/drugs-ozempic-side-effects
- Delong, C. (2023, February 11). Black box warning. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK538521/
- MNT Medical Network. (2023, February 16). Ozempic (semaglutide). https://www.medicalnewstoday.com/articles/326252
- Ozempic® vs. Other Type 2 Diabetes Treatments | Ozempic® (semaglutide) injection 0.5 mg or 1 mg. (n.d.). https://www.ozempic.com/why-ozempic/diabetes-medicines-comparison.html
- Northrop, A. (2023, August 3). Ozempic For Weight Loss: Side Effects, Risks And More. Forbes Health. https://www.forbes.com/health/body/ozempic-for-weight-loss/%20)
- Kerwin McCrimmon, UCHealth, K. (2023, April 5). Wegovy vs. Ozempic: The truth about new ‘weight-loss’ drugs. Uchealth. https://www.uchealth.org/today/wegovy-vs-ozempic-the-truth-about-new-weight-loss-drugs/#:~:text=If%20you%20take%20Wegovy%20or,to%20keep%20benefiting%20from%20them
- Stott, R. (2023, August 4). Lawsuit claims Ozempic, Mounjaro labels ‘downplayed severity’ of gastroparesis. Healio Gastroenterology. Retrieved August 11, 2023, from https://www.healio.com/news/gastroenterology/20230804/lawsuit-claims-ozempic-mounjaro-labels-downplayed-severity-of-gastroparesis#:~:text=While%20the%20drug%20label%20for,not%20recommended%20in%20these%20patients.%E2%80%9D
- How Does Gastroparesis Affect People with Diabetes? (2022, August 30). National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/professionals/diabetes-discoveries-practice/how-gastroparesis-affect-people-with-diabetes
- Living Healthy with Diabetes. (2023, March 29). www.heart.org. https://www.heart.org/en/health-topics/diabetes/prevention–treatment-of-diabetes/living-healthy-with-diabetes
- Move more; sit less. (2023, June 22). Centers for Disease Control and Prevention. https://www.cdc.gov/physicalactivity/basics/adults/index.htm#:~:text=Each%20week%20adults%20need%20150,Physical%20Activity%20Guidelines%20for%20Americans.&text=We%20know%20150%20minutes%20of,do%20it%20all%20at%20once
- Good sleep habits. (2022, September 13). Centers for Disease Control and Prevention. https://www.cdc.gov/sleep/about_sleep/sleep_hygiene.html
- Centers for Disease Control and Prevention. (2022, August 1). Food and nutrition insecurity and diabetes. Centers for Disease Control and Prevention. https://www.cdc.gov/diabetes/library/features/diabetes-and-food-insecurity.htm
- American Psychiatric Association. (2020, December). What is a substance use disorder? https://www.psychiatry.org/patients-families/addiction-substance-use-disorders/what-is-a-substance-use-disorder
- Durrani M, Bansal K. Methadone. [Updated 2023 Apr 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK562216/
- Kumar R, Viswanath O, Saadabadi A. Buprenorphine. [Updated 2023 Apr 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459126/
- National Center for Drug Abuse Statistics. (2023). Drug abuse statistics. https://drugabusestatistics.org/
- National Institute of Health. (2018, June). Understanding drug use and addiction. https://nida.nih.gov/publications/drugfacts/understanding-drug-use-addiction
- Singh D, Saadabadi A. Naltrexone. [Updated 2023 May 30]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK534811/
- Substance Abuse and Mental Health Services Administration. (2023, August). Methadone take-home flexibilities extension guidance. https://www.samhsa.gov/medications-substance-use-disorders/statutes-regulations-guidelines/methadone-guidance#:~:text=In%20treatment%200%2D14%20days,be%20provided%20to%20the%20patient
- S. Food and Drug Administration. (2023, May). Information about medication assisted treatment (MAT). https://www.fda.gov/drugs/information-drug-class/information-about-medication-assisted-treatment-mat
- Akbari, P., Khorasani-Zadeh, A. (Updated 2023, January 23). Thiazide Diuretics. In Stat Pearls. Stat Pearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK532918/
- Alley, W.D., & Schick, M.A. (Updated 2023, July 24). Hypertensive Emergency. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK470371/
- American Heart Association. (2023 June 7). Types of Blood Pressure Medications. Retrieved from https://www.heart.org/en/health-topics/high-blood-pressure/changes-you-can-make-to-manage-high-blood-pressure/types-of-blood-pressure-medications
- Arumugham, V.B., & Shahin, M.H. (Updated 2023, May 29). Therapeutic Uses of Diuretic Agents. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK557838/
- Brater, D.C., & Ellison, D.H. (Updated 2022, November 30). Mechanism of action of diuretics. UpToDate. Retrieved from https://www.uptodate.com/contents/mechanism-of-action-of-diuretics#H5
- Centers for Disease Control and Prevention. (2023, July 6). Facts about Hypertension. Retrieved from https://www.cdc.gov/bloodpressure/facts.htm
- Centers for Disease Control and Prevention. (2021, May 18). High Blood Pressure Symptoms and Causes. Retrieved from https://www.cdc.gov/bloodpressure/about.htm
- Farzam, K., & Jan, A. (Updated 2023, August 22). Beta Blockers. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK532906/
- Goyal, A., Cusick, A.S., & Thielemier, B. (Updated 2023, June 26). ACE Inhibitors. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK430896/
- Hariri, L., & Patel, J.B. (Updated 2023, August 14). Vasodilators. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK554423
- Hill, R.D., & Vaidya, P. (Updated 2023, March 27). Angiotensin II Receptors Blockers (ARBs). In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK537027/
- Huxel, C., Raja, A., Ollivierre-Lawrence, M.D. (Updated 2023, May 22). Loop Diuretics. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK546656/
- LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-. Loop Diuretics. [Updated 2021 Oct 13]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK548619/
- Mann, J.F.E, &Flack, J.M. (Updated 2023, June 22). Choice of Drug Therapy in Primary (Essential) Hypertension. UpToDate. Retrieved from https://www.uptodate.com/contents/choice-of-drug-therapy-in-primary-essential-hypertension
- McKeever, R.G., & Hamilton, R.J. (Updated 2022, August 5). Calcium Channel Blockers. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK482473/
- MedlinePlus. (2023). Hydrochlorothiazide. National Institutes of Health. Retrieved from https://medlineplus.gov/druginfo/meds/a682571.html
- MedlinePlus. (2023). Metoprolol. National Institutes of Health. Retrieved from https://medlineplus.gov/druginfo/meds/a682864.html
- Nachawati D, Patel JB. (Updated 2023, July 3). Alpha-Blockers. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK556066/
- Naranjo, M., Chauhan, S., & Paul, M. (Updated 2023, June 19). Malignant Hypertension. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK507701
- Taylor, B.N., & Cassagnol, M. (Updated 2023, July 10). Alpha-Adrenergic Receptors. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK539830/
- Verdecchia, P., Cavallini, C., & Angeli, F. (2022). Advances in the Treatment Strategies in Hypertension: Present and Future. Journal of cardiovascular development and disease, 9(3), 72. https://doi.org/10.3390/jcdd9030072
- American Academy of Neurology. (2019). AAN Updates Guideline on Valproate for Women with Epilepsy. Neurology Today, 19(5), 46-47.
- American Headache Society. (2020). The American Headache Society position statement on integrating new migraine treatments into clinical practice. Headache: The Journal of Head and Face Pain, 60(3), 415-423.
- American Nurses Association. (2017). Nursing: Scope and standards of practice (3rd ed.). Silver Spring, MD: American Nurses Association.
- Ashina, M., Goadsby, P. J., Reuter, U., Silberstein, S., Dodick, D. W., Xue, F., … & Trugman, J. M. (2020). Long-term efficacy and safety of erenumab in migraine prevention: Results from a 5-year, open-label treatment phase of a randomized clinical trial. European Journal of Neurology, 27(6), 1058-1067.
- Buse, D. C., Silberstein, S. D., Manack, A. N., Papapetropoulos, S., & Lipton, R. B. (2019). Psychiatric comorbidities of episodic and chronic migraine. Journal of Neurology, 266(3), 634-646.
- Davies, N. M., & Anderson, K. E. (2020). Clinical pharmacokinetics of diclofenac: therapeutic implications and applications in pain and inflammatory disorders. Clinical Pharmacokinetics, 59(2), 153-162.
- Dodick, D. W. (2018). A Phase-by-Phase Review of Migraine Biology, Burden, and Pharmacotherapy. Headache: The Journal of Head and Face Pain, 58(S1), 4-16.
- Dodick, D. W., Lipton, R. B., Ailani, J., Lu, K., Finnegan, M., Trugman, J. M., & Szegedi, A. (2019). Ubrogepant for the treatment of migraine. New England Journal of Medicine, 381(23), 2230-2241.
- Dodgson, S. J., Shank, R. P., & Maryanoff, B. E. (2018). Topiramate as an inhibitor of carbonic anhydrase isoenzymes. Epilepsia, 39(12), 16-22.
- D’Souza, P., Himme, A., & Herndon, C. M. (2020). Migraine headache prophylaxis. American Family Physician, 101(5), 297-298.
- Edvinsson, L., & Warfvinge, K. (2019). Recognizing the role of CGRP and CGRP receptors in migraine and its treatment. Cephalalgia, 39(3), 366-373.
- Gomez, M., & Turner, D. (2020). Tailoring Migraine Medications: A Comprehensive Approach. Journal of Neuropharmacology, 15(4), 201-215.
- Gormley, P., Anttila, V., Winsvold, B. S., Palta, P., Esko, T., Pers, T. H., … & Chasman, D. I. (2016). Meta-analysis of 375,000 individuals identifies 38 susceptibility loci for migraine. Nature Genetics, 48(8), 856-866.
- Gupta, R., & Silberstein, S. D. (2020). Migraine and its impact on daily functioning. Headache: The Journal of Head and Face Pain, 60(3), 572-585.
- Headache Classification Committee of the International Headache Society (IHS). (2018). The International Classification of Headache Disorders, 3rd edition. Cephalalgia, 38(1), 1-211.
- Johnson, A., & Davis, R. (2022). Triptans: Mechanisms of Action and Clinical Applications. Headache Medicine Review, 18(2), 87-104.
- Johnson, M., et al. (2022). Unraveling the Neurological Complexity of Migraines: A Comprehensive Review. Neurological Insights, 12(3), 112-129.
- Jones, A. B., & Brown, C. D. (2019). Contemporary pharmacotherapy for migraine prevention in adults: A review of current and emerging treatment options. Drugs, 79(11), 1223-1238.
- Jones, B., & Miller, S. (2022). Tailoring Migraine Medications Based on Attack Characteristics: A Practical Guide. Neurological Insights, 17(3), 211-228.
- Jones, B., et al. (2021). Emerging Trends in Migraine Pharmacotherapy: A Comprehensive Review. Neuropharmacological Insights, 25(3), 312-328.
- Lee, C. R., Bottiglieri, T., Fisher, W. G., La Du, B. N., & Stamer, W. D. (2019). Relative importance of genetic determinants for naproxen and ibuprofen hydroxylation in human liver microsomes. Clinical Pharmacology & Therapeutics, 105(1), 131-140.
- Linde, K., Allais, G., Brinkhaus, B., Manheimer, E., Vickers, A., & White, A. R. (2016). Acupuncture for the prevention of tension‐type headache. Cochrane Database of Systematic Reviews, 2016(4).
- Lipton, R. B., Goadsby, P. J., Smith, J., Schaeffler, B. A., Biondi, D. M., Hirman, J., … & Tepper, S. J. (2019). Efficacy and safety of eptinezumab in patients with chronic migraine: PROMISE-2. Neurology, 92(15), e1705-e1716.
- Lipton, R. B., Hutchinson, S., Ailani, J., Reed, M. L., Fanning, K. M., Manack Adams, A., … & Aurora, S. K. (2017). Discontinuation of acute prescription medication for migraine: Results from the Chronic Migraine Epidemiology and Outcomes (CaMEO) study. Headache: The Journal of Head and Face Pain, 57(10), 1655-1668.
- MaassenVanDenBrink, A., De Vries, T., Danser, A. H., & Headache Expert Panel of the European Academy of Neurology. (2019). Pathophysiology of migraine: a disorder of sensory processing. Physiological Reviews, 99(2), 901-968.
- Miller, S., Johnson, J., & Patel, J. (2021). Ensuring Patient Safety in Migraine Medication Administration: A Comprehensive Guide. Journal of Neurological Nursing, 43(2), 67-78.
- Mims, M. (2021). Mims Medical Microbiology and Immunology. Elsevier Health Sciences.
- Ong, C. K., Seymour, R. A., Lirk, P., Merry, A. F., & Combet, E. (2017). An evidence‐based update on nonsteroidal anti‐inflammatory drugs. Clinical Medicine & Research, 15(2), 73-100.
- Ong, J. J., De Felice, M., & Migraine Pathophysiology, Treatment, and Prevention. (2020). Migraine: Mechanism of action and treatment. The Scientific World Journal, 2020.
- Perucca, P. (2018). Pharmacokinetic variability of new antiepileptic drugs at different ages. Therapeutic Drug Monitoring, 40(6), 723-733.
- Serrano, D., Lipton, R. B., Scher, A. I., Reed, M. L., Stewart, W. F., & Adams, A. M. (2015). Fluctuations in episodic and chronic migraine status over the course of 1 year: Implications for diagnosis, treatment and clinical trial design. Journal of Headache and Pain, 16(1), 1-12.
- Silberstein, S. D., Holland, S., Freitag, F., Dodick, D. W., Argoff, C., Ashman, E., … & Quality Standards Subcommittee of the American Academy of Neurology and the American Headache Society. (2019). Evidence-based guideline update: pharmacologic treatment for episodic migraine prevention in adults. Neurology, 92(18), 1-12.
- Smith, J., & Patel, S. (2023). Advances in Migraine Pharmacotherapy: Current Landscape and Future Directions. Neurology Today, 19(1), 45-62.
- Smith, R. H., et al. (2020). Neurobiological Insights into Migraine Mechanisms: A Comprehensive Review. Neurology Research International, 2020, 8743521.
- Smith, J., et al. (2021). Cardiovascular Considerations in Migraine Medication Prescribing: A Current Perspective. Current Neurology and Neuroscience Reports, 21(5), 15.
- Smith, S. M., Gums, J. G., & Potti, A. (2021). Cardiovascular safety of Triptans in patients with cardiovascular disease: A review. The American Journal of Medicine, 134(2), 146-154.
- Tepper, S. J., & Ashina, M. (2020). Reuter U. Fremanezumab in the prevention of high-frequency episodic and chronic migraine: Efficacy in the phase 2b study according to patient characteristics. The Journal of Headache and Pain, 21(1), 23.
- Tepper, S. J., & Cady, R. K. (2019). Diagnosis and Management of Acute Migraine. Disease-a-Month, 65(4), 100856.
- Tepper, S. J., & Diener, H. C. (2020). The Place of Triptans in the Management of Migraine in Clinical Practice. Cephalalgia, 40(2), 155-166.
- Tiseo, C., Vacca, G., & Pinzi, C. (2020). Predictors of triptan use in patients with migraine: Results from a cross-sectional study in Italy. PLoS ONE, 15(7), e0235568.
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate
