Course
Florida Laws and Regulations
Course Highlights
- In this Florida Laws and Regulations course, we will learn about Florida Laws and regulations, and why it is important to abide by them.
- You’ll also learn the basics of stipulations and documentation, as required by the Florida Board of Nursing.
- You’ll leave this course with a broader understanding of license renewals, and violations of practice acts.
About
Contact Hours Awarded: 2
Course By:
Kayla M. Cavicchio
BSN, RN, CEN
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
The state of Florida has several statutes that govern the practice of nurses. These statutes consist of Chapters 456 and 464 in Title XXXII Regulation of Professions and Occupations. The Florida Administrative Code is where Division 64B9 is located.
Chapter 464, often called the Nurse Practice Act, is separated into two parts. Part I discusses the advanced practiced registered nurse, registered nurse, and licensed practical nurse. This statute ensures that every nurse practicing in Florida is held to and meets the same minimum standards for safe practice.
Because of this, nurses who do not meet the minimum requirements or display harm to society are not allowed to practice nursing in the state of Florida. The Board of Nursing is the governing body for the Nurse Practice Act and deals with matters such as providing licensure, creating rules, and managing disciplinary actions. Part II of chapter 464 focuses on the certified nursing assistant.
Chapter 456 is a statute directed at all healthcare providers and professions. This statute lists the provisions that Chapter 464 is built on.
Division 64B9 is part of the Florida Administrative Code that provides specific rules that pertain to nurses and how the profession is regulated in terms of eligibility to take the examination of selected practice, set standards for nursing education curriculum and institutions, continuing education requirements, license renewal; rules for impairment of the nurse in the workplace and more.
This course is designed to meet the requirements of Division 64B9-5 as it pertains to two continuing educational hours about Florida’s laws and regulations of nursing practice.

Definitions (3, 4, 5)
Advanced or specialized nursing practice — completion of post-basic specialized training, experience, and education that are appropriately performed by an advanced practice registered nurse. The advanced-level nurse can “perform acts of medical diagnosis and treatment, prescription, and operation” under the authorization of a protocol with the supervision of a physician.
Advanced practice registered nurse (APRN) — any individual who is licensed in this state to practice professional nursing as defined above and holds a license in advanced nursing practice, including:
- Certified Nurse Midwives (CNM or nurse midwife)
- Able to perform superficial or minor surgical procedures as defined by a protocol and approved by the employing medical facility or with a backup physician in the case of a home birth.
- Start and perform approved anesthetic procedures.
- Order appropriate medications based on patient and condition.
- Manage care of the normal obstetrics patient and the newborn patient.
- Certified Nurse Practitioners (CNP)
- Able to manage some medical issues guided by facility or supervising provider protocols.
- Manage and monitor patients who have stable, chronic illnesses.
- Start, monitor, and adjust therapies for select, uncomplicated illnesses.
- Order occupational and physical therapy based on patient needs.
- Certified Registered Nurse Anesthetists (CRNA)
- Able to order pre-anesthetic medications as stated and approved by facility protocols and staff.
- Determine and consult with the supervising anesthesiologist about the proper anesthesia for patients based on labs, history, and physical and patient conditions.
- Assist with managing the patient in the post-anesthesia care unit.
- Clinical Nurse Specialists (CNS)
- A nurse prepared in a CNS-focused program that meets the requirements of a typical APRN program. Additionally, they are trained in the area of expertise that pertains to the advanced practice of nurses.
- Psychiatric Nurse
- Has a master’s or doctoral degree in psychiatric nursing and has a national advanced practice certification as a psychiatric mental health advanced practice nurse.
- has two years of post-master's clinical experience under the supervision of a physician.
- They can prescribe psychotropic controlled substances for the treatment of mental health disorders.
Board — the Board of Nursing.
Licensed Practical Nurse (LPN) — any person licensed in this state or holding an active multistate license under s. 464.0095 to practice practical nursing as defined below.
Practice of practical nursing — the performance of select actions, including the management of specific treatments and medications, while taking care of the ill, injured, or infirm; prevention of illness, promotion of wellness, and health maintenance in others under the direction of a registered nurse, or a licensed provider: physician, osteopathic physician, podiatric physician, or dentist; and the teaching of general health principles and wellness to the public and students other than nursing students. A practical nurse is responsible and accountable for making decisions based on their educational preparation and experience in the profession.
Practice of professional nursing — the performance of actions requiring substantial specialized knowledge, judgment, and nursing skill based on applied principles of physical, psychological, social, and biological sciences, which shall include, but are not limited to:
- The nursing process consists of assessment, nursing diagnosis, planning, intervention, and evaluation of care; teaching and counseling of the ill, injured, or infirm in matters of health; prevention of illness, promotion of wellness, and maintenance of the health of others.
- The administration of medications and treatments as prescribed or authorized by a duly licensed practitioner as they are authorized to do so by the laws of this state to prescribe such medications and treatments.
- The management and education of other individuals, such as nursing students, in the theory and performance of any of the acts described above.
A professional nurse is responsible and accountable for making decisions based on the individual's educational preparation and experience.
Registered nurse (RN) — means any person licensed in this state or holding an active multistate license under s. 464.0095 to practice professional nursing as defined above.
A registered nurse first assistant (RNFA) — is a registered nurse who assists in surgery while in the hospital setting under a physician. They help maintain cost-effective and quality surgery for patients in Florida. They must be certified in perioperative nursing via a core curriculum approved by the Association of Operating Room Nurses, Inc.

Self Quiz
Ask yourself...
- What license or licenses do you currently hold? Have you held another permit in the past?
- What other licensed nursing providers do you work with at your facility?
- What type of APRN license listed in the above definitions surprised you the most? Why?
- Do you agree with the definitions of practical nursing and professional nursing? What is your rationale?
Board of Nursing: Members and Headquarters Location
Florida’s Board of Nursing has 13 unique members that Florida's governor appoints. To maintain diversity and representation of the entire nursing profession, the following criteria must be met (5):
- Seven members must be RNs with a minimum of four years of experience in practice.
- One must be an APRN
- One must be a nurse educator
- One must be a nurse executive
- Three members must be LPNs with a minimum of four years of experience in practice.
- The final three members have no connection to the nursing profession or affiliation or contract with a healthcare agency.
- One member must be over the age of 60
- All members must be residents of the state of Florida
Membership terms last for four years; however, if the governor does not have a successor to appoint, the members can serve for another four years. The Board of Nursing's headquarters is in Tallahassee per Florida statute (5).
The members of the Board have several roles and responsibilities while serving. Their primary job is to ensure that nurses practicing in Florida are doing so safely. To do this, the Board members can create and implement rules or provisions to add to the Nurse Practice Act.
They can approve educational programs for institutions wishing to teach nursing. They can take disciplinary action against a nurse for violating the Nurse Practice Act or other Florida laws. Disciplinary actions can consist of citations, fines, or disciplinary guidelines based on the nurse in question, previous offenses, and the severity of the violation. (5).
Licensure by Examination and Endorsement
Initial licensure requires an individual to examine their desired profession: NCLEX-RN, NCLEX-LPN, and either the American Nurses Credentialing Center (ANCC) or the American Association of Nurse Practitioners (AANP) version for those wishing to become an APRN. In order for the Board of Nursing to approve an individual to sit for their desired examination, a list of requirements must be met in total (5):
- You must correctly complete an application for the desired examination and submit a fee set by the Board.
- Submit to a background check conducted by the Department of Law Enforcement.
- Must be in good physical and mental health and receive a high school diploma or equivalent.
- Has completed the following requirements:
- Graduate from an approved program on or after July 1, 2009, OR
- Graduate from a prelicensure nursing education program that has been determined to be equivalent to an approved program by the Board before July 1, 2009
- Must have the ability to communicate effectively in English as determined by the Department of Health through another examination as indicated.
It is important to note that there is a section dedicated to the scenario of an individual failing the examination or needing to take it within six months of graduating.
Candidates can take the test up to three times if they fail it. Suppose an individual needs to pass their examination of choice after three attempts. In that case, they must take a Board-approved remediation course before they can sit for the examination again. From there, they are given three more chances to take and pass the test before they must remediate again. Reexamination must occur within six months of the approved remediation course (5).
If an individual fails to take their examination within six months of graduation, they must take an exam preparation course approved by the Board. It is to be advised that the individual must pay for the course without using federal or state financial aid (5).
Courses completed in a professional nursing education program that are at least equivalent to a practical nursing education program may be used to satisfy the education requirements for licensure as a licensed practical nurse. This means a registered nursing program student could take the licensure for an LPN license once the courses they have taken meet the LPN licensure requirements (5).
If a nurse holds licensure in another state or US territory and decides to obtain Florida licensure, theycan do so through endorsement. Florida requires those who apply to submit a nonrefundable fee, complete the application, and provide fingerprints for a criminal background check. The Florida Board of Nursing will not issue a license to an individual under investigation when applying (5).
Military Spouses
Applying for a license through endorsement is a route that can be used for nurses who are traveling with military spouses on official military orders. Nurses must have actively practiced nursing for two of the three years before applying for a license. Military spouses also have the option of obtaining a 12-month temporary Florida license if they meet the requirements (4):
- Holds a valid nursing license in another state
- Has a negative criminal background check
- Has not failed their licensure exam
- Has not had any disciplinary action taken against them in another state
Licensure by Compact
Over 40 states in the United States have created legislation to allow nurses to work under one multistate license (2). This means a nurse originally licensed in Florida could work in any other state that participates in the Nurse Licensure Compact without obtaining licensure for each state they wish to work in if they have a multistate license. This has proven especially useful over the years due to the growing nursing shortage and global pandemic.
Many states like Florida are offering to provide multistate licenses to nurses during their initial examination. If a nurse does not obtain a multistate license initially, they can do so later. They must pay a fee and submit fingerprints for a background check. Nurses must also meet any other requirements set by the state of Florida (2).
It is important to note that in Florida, the nurse who holds the compact license must claim residency in the state. If the nurse were to claim residency in another state, they would no longer have a multistate license issued by Florida. If the state they move to is part of the Nurse Licensure Compact, they might be eligible to obtain a compact license in their new home state (2, 5).
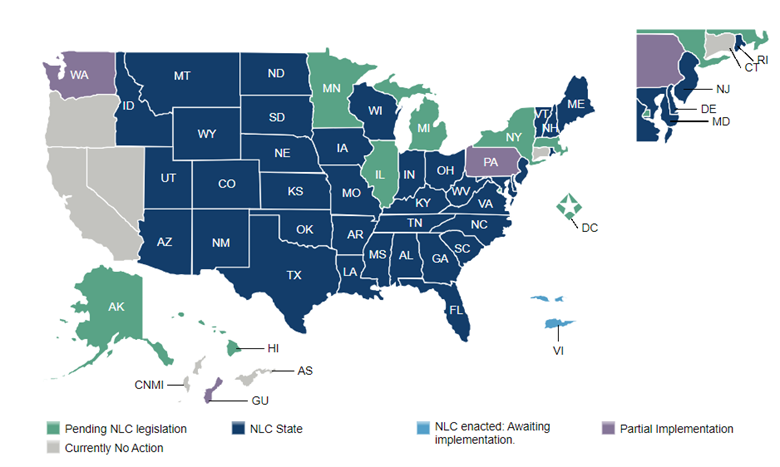
(2)

Self Quiz
Ask yourself...
- Do you feel as though Florida’s Board of Nursing has a diverse nursing population?
- Who should appoint members to the Board?
- What information were you required to provide to the Board of Nursing when you applied to take your licensure exam?
- Have you obtained licensure through endorsement, whether in Florida or another state?
- When do you anticipate nurses being able to practice in all 50 states and US territories? Will this be beneficial to healthcare? Why or why not?
Delegation to the Unlicensed Assistive Personnel (UAP) or Unlicensed Personnel (UP)
The Nurse Practice Act defines delegation as transferring a task or activity during a specific situation by a qualified nurse, through licensure and experience in the task, to a competent individual. Different facilities may have several ways of determining the competence of the individuals they employ, but ultimately, the decision rests with the RN or LPN.
The licensed provider must evaluate the task's difficulty, the potential for predictable or unpredictable harm or rapid change in the patient's condition, and the level of communication required with the patient. They must also consider the resources available and skills the UAP can do at their facility (4).
When delegating, it is essential to assess the UAP's skill set through validation or verification. The nurse should communicate clearly regarding the delegated task and explain the desired outcomes. They should also explain what undesired outcomes could occur, what should be done if an undesired outcome does happen when the task should be completed, and if supervision by the nurse is required.
The nurse should follow up to ensure the task was done correctly and within the set time frame. The nurse should be aware that the delegated task and any outcomes are the nurse's responsibility, and they are ultimately held accountable for it. So, if it is an important task, it may be in the best interest of the nurse to delegate another task to the UAP and perform the critical task themselves (4).
There are a few skills that cannot be delegated to the UAP:
- A skill that is not within the delegating nurse’s scope of practice
- Activities require using the nursing process or specific education, judgment, training, or skills.
- Initial assessments and progress evaluations relate to the patient's plan of care.
- Skills that a UAP needs to display competence.
IV Administration by LPNs
As mentioned above, LPNs and RNs have a few variations in their scope of practice. LPNs can administer and perform some parts of IV medication therapy instead of the RN, who can do all. IV therapy administration is the infusion or injection of a medication via the intravenous system.
This method involves several aspects, including evaluating, observing, monitoring, discontinuing, titrating, managing, planning, documenting, and intervening during administration. RNs do not always have to be onsite when delegating IV administration to an LPN, but knowing policies and when an RN must be on site is essential (4).
LPNs cannot do any of the following (4):
- Initiate blood or blood products or plasma extenders.
- Mix IV solutions.
- Administer or initiate cancer treatments such as chemotherapy or investigational medications.
- IV pushes, except for heparin or saline flushes.
LPNs may care for patients receiving these therapies, such as actively receiving a blood transfusion, but they cannot do the above.
LPNs can (4):
- Calculate and adjust flow rates.
- Observe and report any signs of adverse effects of IV medications.
- Assess IV insertion sites and change dressings as needed and as educated.
- Remove IV catheters or needles from peripheral veins.
- Hang IV hydrating fluids.
In order for an LPN to administer IV medications through a central line, they must do so under the direction of an RN and have four hours of IV therapy education on central lines. This four-hour requirement can be applied to the 30 total hours LPNs must do on IV therapy (4).
LPN Supervision in Nursing Homes
According to Florida law, LPNs can supervise other LPNs, certified nursing assistants (CNAs), or UAPs in the nursing home setting. To be considered for a supervisory position, the LPN must have completed 30 hours of board-approved, post-basic education courses under the supervision of an RN.
The LPN must also have at least six months of full-time clinical experience either in a hospital or nursing home setting. If the LPN takes a course outside of the Board’s approval courses, the provider of said course must test the LPN and provide attestation of the LPN’s competency (4).
The supervisory LPN's role is to provide other LPNs, CNAs, and UPAs with guidance and inspection of their completed task per their appropriate scope of practice. The LPN can only delegate tasks within their scope of practice and be assured that the one they are delegating to demonstrates competency (4).
Certified Nursing Assistant (CNA)
The certified nursing assistant is similar to the UAP. Still, to be certified, they must have completed a background check conducted by the Board of Nursing, prove they can read and write, and pass the nursing assistant examination. Once the criteria listed have been met, CNAs can provide general care and assist with activities of daily living under the direction of an RN or LPN. They can also participate in postmortem care and perform CPR (4).

Self Quiz
Ask yourself...
- Think of your facility or organization: what types of UAPs do you have? CNAs, Patient Care Technicians (PCTs), emergency service technicians?
- Are you aware of what you can and can’t delegate to them?
- Are there any LPNs where you work?
- What can they do, and what types of patients can they care for?
- Some acute care facilities have started to wean out the LPN role while others are hiring them to address short-staffing needs within their organizations. What do you think of these decisions and which do you prefer?
Maintaining Medical Records
For RNs and APRNs in private practice, the Florida Nurse Practice Act has two rules regarding maintaining medical records. The first applies to the death of the nurse. Whoever legally represents the RN or APRN must post a notification in the county newspaper stating where the medical records are being stored and who to contact if an individual wants to obtain the records. The documents must be stored for a minimum of two years after the death of the nurse (4).
At the 24-month mark, several notices must be posted in the county newspaper, one notification for four consecutive weeks, that the medical records will be destroyed four weeks after the last day of the fourth week that the notice was published (4).
The second rule pertains to an RN or APRN who has terminated or relocated their practice. The rule states that the RN or APRN maintains and holds onto the medical records for at least two years. They must let those who were patients know about the date of termination or relocation and where the medical records can be retrieved.
The notice must be made public, such as in a newspaper, with a minimum appearance of four times over four weeks. A sign must be placed at the location of the business about the termination or relocation until the termination or relocation happens. This sign must tell patients about the opportunity to obtain their medical records (4).
Continuing Education (CE) Requirements
Florida law requires that for renewal of a nursing license, the nurse seeking renewal must complete a set amount of CE hours. Over the two years, 24 hours must be completed, one for each month. Two of those hours must be about the Florida Nurse Practice Act and the other laws that pertain to the nursing profession.
Two hours are required to investigate medication errors and how to prevent them. A one-hour HIV/AIDS is necessary for initial renewal but does not have to be repeated. There must be a two-hour course on domestic violence done every third renewal. As of August 2017, a two-hour course on recognizing impairment in the workplace is required with each renewal (4).
In Florida, completed CE courses are automatically reported to a tracking system created by the Department of Health’s Division of Medical Quality and Assurance (MQA) or manually by the individual. Those who attend CE courses will obtain a certificate of attendance. The attendee is advised to maintain a copy of those certificates for at least four years.
For Florida, the provider of the course, the individual or company that is offering the training, has 90 days (about 3 months) to report to the tracking system, so if the nurse’s date of renewal is less than 90 days, it is suggested that the course be manually reported by the nurse (4).
If a nurse has two licenses, such as RN and LPN or APRN and RN, they may be able to comply with both license requirements through one set of CE requirements. For example, an RN with an LPN license can meet all the CE requirements of the LPN license by completing the RN requirements (4).
Nurses who serve as expert witnesses and provide expert opinions in writing can obtain 2.5 hours for each case. The case must cite at least two current articles of reference being reviewed regarding the Nurse Practice Act (4).
There are a few exemptions to completing the CE renewal requirements. It is advised that the nurse contact the Board of Nursing with specific questions or concerns regarding renewal and CE requirements (4):
- If the nurse is on active duty for the US military within six months of the renewal date.
- This does not apply to short periods of active duty, such as summer or weekend drills.
- This does not apply to those on duty in the US Public Health Service.
- If the nurse’s spouse is a member of the US military and the nurse was absent from the state of Florida because of military duty.
- The nurse must provide adequate proof of the spouse's absence and military status.

Self Quiz
Ask yourself...
- What types of classes do you take to complete your continuing education? Online, in-person, webinar? Which one do you like the best?
- What Florida-mandated classes do you have the most challenging time finding and completing?
- Do you hold licenses in two aspects of nursing, such as LPN and RN, or RN and APRN? If so, how do you complete both your continuing education requirements?
- Do you use a CE tracking site to ensure you are compliant with your CEs? What are the pros and cons of using it?
Disciplinary Action
As mentioned above, the Florida Board of Nursing, as outlined in the Nurse Practice Act, can discipline nurses as they see fit regarding all violations of Florida rules and laws. The Board created a variety of ways a nurse can be punished, ranging from probable-cause panels to citations to disciplinary hearings to loss of nursing license. The severity of the violation reflects on which method the Board of Nursing may take (5).
There are three probable-cause panels in Florida: North Florida, Central Florida, and South Florida. The purpose of these panels is to determine if there was “probable cause” or reasonable ground for the reported case. They decide if a case needs action taken. The panel members review each case and compare it to others of a similar nature, how the Board has treated those cases in the past and what the Board's guidelines entail. The panel can recommend and consider rules regarding procedures, penalties, and disciplinary actions (5)
Citations can be given in lieu of other forms of discipline. The citation is issued within six months of a complaint being filed and contains the request for the recipient to fix the violation within a specified time frame. These violations are usually classified as “minor” in nature, such as false advertising, falsely using a nursing title, or failure to report the change of address or updates of information required by the Board.
Other reasons a citation can be issued include failing to report a misdemeanor within 30 days of a ruling or failing to utilize the law-required prescription drug monitoring system. Each of these citations can come with a fine, usually ranging from $100 to $250 in amount; however, if a nurse is found guilty of sharing passwords, codes, keys, or other forms of entry to a secure medication administration device or information technology system a fine of $1,500 can be given. In addition, the nurse would have to take a two-hour CE course on legal nursing aspects within 60 days of the citation being issued (5).
The Board of Nursing has the power to take any of the below appropriate actions against nurses who have violated parts of the Nurse Practice Act. It is important to note that any of the actions can be combined, depending on the severity of the violation and the action taken by the nurse after the violation was committed (5):
- Probation, suspension, or revocation of a license
- It can be emergently done depending on the situation.
- Require CE course(s) to be done
- Letter of concern
- Reprimand
- Administer a fine
- A personal appearance is required before the Board of Nursing to monitor compliance.
- Restrict or limit a nurse's scope of practice.
- Example: prohibiting a nurse from administering any narcotics after they are participating in drug diversion
- Referral to the Intervention Project for Nurses (IPN)
The Board of Nursing has also created an extensive, but not all-encompassing list of reasons why a nurse can be disciplined (5):
- Sexual misconduct
- Unprofessional conduct
- Participating in crime related to healthcare fraud
- Making or filing a false report to appease state or federal law
- Willfully hindering another individual in filing a report that is required by state or federal law
- Testing positive on any drug screen when the individual has no medical/other reason for using the drug
- Inability to practice nursing with satisfactory skill and provide safe patient care due to the use of narcotics, drugs, alcohol, chemicals, or other substances that may impair an individual
- Inability to practice nursing with satisfactory skill and provide safe patient care due to an illness, physical or mental condition
- Failing to meet minimal standards of acceptable nursing practice
- Accepting and performing professional responsibilities the nurse knows or has reason to know they are not skilled to perform
- Delegating or contracting for the performance of professional duties by a person who the nurse knows or has reason to know is not qualified by training, experience, and authorization required to perform
- Failing to identify the type of license the nurse is practicing under through written (can include a nametag) or oral notice to a patient
- Performing or attempting to perform healthcare services on the wrong site or the wrong procedure on the wrong patient includes unauthorized procedures
- Performing or attempting to perform healthcare services that are medically unnecessary or otherwise not related to the patient’s diagnosis or medical condition(s)
- Being convicted or found guilty of or pleading nolo contendere (no contest) to a crime in any jurisdiction that directly relates to the practice of nursing or the ability to practice nursing
- Being convicted of or found guilty of, or pleading nolo contendere to misdemeanors related to failure to protect an adult from abuse, neglect, and exploitation; fraudulent practices; theft and robbery; or having committed an act of domestic violence or child abuse
- Defaulting on a student loan that has been issued or guaranteed by the state or federal government
As with everything in life, the Board of Nursing has created guidelines for imposing discipline. They have a set minimum and maximum amount when it comes to fines. They have time frames for probation or supervision, conditions regarding probation, or the reinstatement of a license. What route they decide to take depends upon the specific case being presented to them. Sometimes, the circumstances presented to the Board are enough to elicit decisions outside the general guidelines. Some of these circumstances are (5):
- Length of time a nurse has practiced
- Presents a danger to the public
- Any visible effort at rehabilitation
- Treatment and disciplinary hearing costs
- Actual physical or other forms of damage caused by the nurse
- Financial hardships
The Board has a timeframe in which a complaint must be filed. Most of the time, it is within a six-year window from the time the incident occurred. However, in certain circumstances—criminal actions, sexual misconduct, impairment of the nurse, or usage/diversion of controlled medications—the Board may allow the complaint’s time frame to extend beyond the six-year timeframe.
Suppose action such as fraud, intentional misrepresentation, or concealment is utilized to hide the violation during the six years. In that case, the timeframe to file a complaint can be extended to 12 years from when the incident occurred (5).
If the Board of Nursing suspends a nurse's license or agrees to have the license suspended to avoid further action against them, the nurse can possibly file a petition to have their license reinstated. Any final orders or terms issued during the initial suspension must be met as a whole, and the nurse must be able to demonstrate the ability to perform nursing practice safely.
Sometimes, a time frame is set for when a nurse can file a petition; sometimes, there is not. If this is the case, a nurse can appeal as soon as they can after meeting the terms and conditions given to them by the Board (5).
The Board will determine what a nurse must do to demonstrate safe practice. This is based on the violation. For example, a nurse who is working while under the influence of medications or alcohol may be ordered to attend a treatment program with proof of sobriety, references, and completion of any court-mandated sanctions. Nurses must often present to the Board of Nursing in person and speak on their ability to practice nursing (5) safely.
The three-strike policy is utilized when it comes to reinstating a license. Suppose a nurse has been found guilty on three separate occasions of a complaint about drug/narcotic usage or the diversion of medications from patients to the nurse for personal use or to sell. In that case, the Board will not reinstate the license (5).
Relicensing a nurse who has had their license revoked is similar to what happens when a license is suspended. However, the nurse must reapply for the permit and meet all conditions set by the Board. Nurses may have to sit for another examination or take board-approved continuing education if the nurse has been out of practice for an extended period of time. They may require a nurse to participate in Florida’s Intervention Project for Nurses (IPN) program or at least be evaluated for it (5).
Nurses are held accountable for reporting the actions of other nurses and any misconduct to the Board of Nursing. They must report sexual misconduct or healthcare fraud. If they know or have reason to believe that another nurse is not practicing safely or is practicing under the influence of alcohol or medications, they are required to report it (5).

Self Quiz
Ask yourself...
- Do you know anyone who has had action taken against them regarding the Nurse Practice Act?
- If so, what was the outcome?
- What other actions do you think could violate the Nurse Practice Act? What other actions outside the Nurse Practice Act should the Board of Nursing address?
- What do you think is the most severe violation listed above?
- Is the Board of Nursing's list of potential actions that could be taken against a nurse's license fair?
- If you were on the Board, what types of disciplinary action would you recommend?
Florida’s Intervention Project for Nurses (IPN)
Created in 1983 under the authority of the Nurse Practice Act, IPN was designed to protect the public by monitoring nurses whose skills have been compromised due to improper use of medications or alcohol or the impairment of mental or physical health. IPN is not a treatment center.
Instead, they provide nurses with access to Board-approved practitioners who specialize in addiction, mental health, and other medical conditions to assist the nurses in restoring themselves to a level of safe practice. They also conduct monitoring after a nurse has been discharged from treatment, interventional training, consultations, and advocacy for those who participate (1).
As mentioned above, nurses have an obligation to report themselves or nurses who are, or they have reason to believe, unsafely practicing nursing while under the influence of alcohol or medications. The report is confidential if a nurse self-reports or is reported to the IPN only and they complete treatment and five years of monitoring. If the Board of Nursing becomes involved, either through a failure to report or complete treatment, disciplinary action may be taken (1).
In the beginning, nurses are not able to practice during the initial evaluation period or when the treatment is being determined. After a treatment plan is made, it is up to the discretion of the IPN and the providers involved in the treatment to say if the nurse is able to continue working as a nurse. Restrictions on a nurse’s practice are often implemented during the beginning phase of treatment(1).
To be determined “fit to practice,” the nurse must meet all requirements set by their providers and the IPN. They must sign an advocacy contract, submit to random drug tests, verbalize their understanding of practice restrictions, and participate in a weekly support group for nurses (1).

Self Quiz
Ask yourself...
- Should the IPN be a treatment center as opposed to a resource center? Should they offer both?
- Should the status of a nurse who has enrolled in this program, willingly or not, be confidential, even if they do not meet the requirements?
- Should a nurse be allowed to practice nursing with set limitations while being involved with an IPN? Why or why not?
- Do you know anyone who was involved in IPN? What were their limitations of practice? Were they successful or not?
Conclusion
Despite the extensive outline of the Nurse Practice Act and other state rules in this course, it only briefly narrates all Florida laws pertaining to nurses. In addition to this course, nurses must stay on top of new legislation being proposed and implemented regarding their profession and continually review the content in the state laws. Nurses who travel to other states to practice their profession should be educated on each state’s rules regarding nursing practice, as they can differ from state to state. A conscious effort must be made to follow the laws set in place to practice nursing safely and legally in the state of Florida.
References + Disclaimer
- Intervention Project for Nurses. (2024). About. Intervention Project for Nurses. https://www.ipnfl.org/about/
- National Council of State Boards of Nursing. (2024). Participating jurisdictions. NURSECOMPACT. https://www.nursecompact.com/
- The Florida Senate. (2023a). Chapter 394, section 455. Www.flsenate.gov. https://www.flsenate.gov/Laws/Statutes/2023/394.455
- The Florida Senate. (2023b). Chapter 456. Www.flsenate.gov. https://www.flsenate.gov/Laws/Statutes/2023/Chapter456/All
- The Florida Senate. (2023c). Chapter 464. Www.flsenate.gov. https://www.flsenate.gov/Laws/Statutes/2023/Chapter464/PART_I
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate
