Course
Understanding the Types of Anemia
Course Highlights
- In this course we will learn about the various types of anemia and their specific lab values.
- You’ll also learn the basics of red blood cell production.
- You’ll leave this course with a broader understanding of interpretting key lab values that indicate anemia.
About
Contact Hours Awarded: 1.5

Course By:
Ashley Kellish
DNP, RN, CCNS
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Anemia remains a common and complex diagnosis in the healthcare setting. From relative anemias subsequent to fluid overload or dehydration, to true anemia secondary to illness or related to a genetic disorder, a nurse is never far from an anemia diagnosis. That said, we can enhance our ability to describe and determine the various types of anemia based on digging deeper into the lab values that exist with anemia.
Introduction
Anemia, by definition, is a decrease in the concentration of hemoglobin (Hgb) or hematocrit (Hct) in the blood (2). The human body makes 2 million red blood cells (RBCs) per second. The RBC is constantly regulated by blood concentration passing through the kidneys (2). When the hemoglobin is low, the kidneys secrete a hormone called erythropoietin. This hormone sends a message to the bone marrow to produce more RBCs. Several types of anemia have various causes, including nutritional deficiencies, hereditary causes, pregnancy, or blood loss (1).
Our body requires nutrients like iron (needed for the synthesis of hemoglobin), B12, folate, B6, riboflavin, pantothenic acid, niacin, ascorbic acid, and vitamin E to make and maintain an adequate number of RBCs. Deficiencies in these elements can cause certain types of anemia (2).
Two crucial nutrients, folate and B12, are absorbed from food in the gut and are integral in the production and maturation of RBCs. Folate and B12 deficiencies lead to impaired DNA synthesis in the bone marrow during RBC production. Cells that lack folate and B12 are larger than normal RBCs because they are immature cells that do not have the nutrients they need to become fully formed and functional (5). When iron is deficient in the body, RBCs will appear smaller than usual (2).
RBC Production
RBCs are produced in bone marrow (2). Pluripotent stem cells differentiate into either myeloid or lymphoid stem cells. Lymphoid stem cells differentiate further into lymphocytes, while myeloid cells differentiate into erythrocytes, thrombocytes, granulocytes, and macrophages. Erythrocytes are what eventually become RBCs. Interestingly, when an erythrocyte differentiates into a reticulocyte or immature RBC, this is what is initially released into the bloodstream (2). At this point, it has no nucleus, which is very different from most cells!
Reticulocytes, or immature RBCs, still have another 24-48 hours of development before they mature into functioning RBCs. During this time, they also lose their mitochondria and ribosomes. They make up 1% of the total RBCs (2).
With these typical cell organelles missing, the RBC makes and uses energy, or ATP, in a very different way than the usual cell. RBCs have a lifespan of 120 days and undergo a very formal destruction process that allows our body to recycle certain parts of the RBC for later use (2, 4).
As an RBC age, enzyme activities decrease, and membrane lipids decrease, allowing for instability due to the rise of destructive elements like HBA and methemoglobin.
When changes in cell size occur, the cell becomes increasingly fragile and is removed by the mononuclear phagocytic system. Approximately 80-90% of this process occurs in the liver and spleen, where the globulin and iron stores can be recycled while the heme is reduced to bilirubin (2, 4 & 5). Bilirubin is broken down into urobilinogen and is excreted in our feces. Increased red cell destruction can be seen as increased serum levels of unconjugated bilirubin and increased excretion of urobilinogen. This can be indicative of hemolytic anemia (3, 6).
Types of Anemia
A variety of factors can cause anemia. Read on below to learn more about each:
Iron Deficiency
Anemia Iron deficiency anemia occurs when the body lacks sufficient iron to produce hemoglobin, the protein in red blood cells responsible for carrying oxygen to tissues. This deficiency often stems from inadequate dietary intake, blood loss (such as from menstruation or gastrointestinal bleeding), or an inability to absorb iron efficiently. Common symptoms include fatigue, weakness, pale skin, shortness of breath, dizziness, and headaches. Diagnosis typically involves blood tests revealing low levels of hemoglobin and serum ferritin. Treatment usually consists of iron supplementation and addressing the underlying cause of the deficiency, with dietary changes and, in some cases, medical interventions to control bleeding or improve iron absorption (7).
Hemolytic Anemia
Hemolytic anemia is characterized by prematurely destroying red blood cells, leading to a shortage of these cells in the bloodstream. This destruction can occur within the bloodstream or in organs such as the spleen or liver. There are various causes of hemolytic anemia, including autoimmune disorders, genetic conditions, infections, certain medications, and exposure to toxins. Common symptoms include fatigue, weakness, jaundice, dark urine, and splenomegaly. Diagnosis involves labs revealing low levels of red blood cells and elevated markers indicating increased red blood cell destruction. Treatment depends on the underlying cause but may include medication, blood transfusions, or, in severe cases, surgical removal of the spleen (7).
Folate Deficiency Anemia
Folate deficiency anemia occurs when the body lacks adequate folate, a B vitamin essential for red blood cell production. This deficiency often results from insufficient dietary intake, malabsorption conditions, increased demand during pregnancy, or periods of rapid growth. Without enough folate, the bone marrow produces larger and fewer red blood cells, leading to anemia. Symptoms include fatigue, weakness, shortness of breath, pale skin, and possible gastrointestinal issues. Diagnosis typically involves blood tests showing low levels of folate and abnormal red blood cell characteristics. Treatment primarily consists of folate supplementation and addressing the underlying cause, such as improving dietary intake or managing malabsorption disorders (7).
Vitamin B12 Deficiency Anemia
Much like folate deficiency anemia, vitamin B12 deficiency occurs when the body lacks sufficient vitamin B12, a vitamin crucial for red blood cell formation and neurological function. This deficiency often stems from inadequate dietary intake and impaired absorption due to pernicious anemia, gastrointestinal disorders, or certain medications. Without enough B12, the bone marrow produces larger and fewer red blood cells, leading to anemia. Symptoms are similar to the ones listed for folate deficiency. Also, they may include fatigue, weakness, pale or jaundiced skin, shortness of breath, tingling or numbness in the hands and feet, and cognitive difficulties. Diagnosis typically involves blood tests revealing low levels of B12 and abnormal red blood cell characteristics. Treatment usually consists of B12 supplementation via injections or oral supplements and addressing the underlying cause (7).
Aplastic Anemia
Aplastic anemia is a rare but severe condition characterized by the failure of the bone marrow to produce enough blood cells, including red blood cells, white blood cells, and platelets. This failure is often due to damage to the bone marrow’s stem cells, which can be caused by factors such as autoimmune disorders, exposure to toxins, certain medications, viral infections like hepatitis or HIV, or inherited genetic conditions. Symptoms of aplastic anemia can vary but often include fatigue, weakness, shortness of breath, pale skin, frequent infections, and easy bruising or bleeding. Diagnosis involves blood tests revealing low levels of all blood cell types and a bone marrow biopsy to confirm the diagnosis. Treatment may include blood transfusions, medications to stimulate blood cell production, immunosuppressive therapy, or, in severe cases, a bone marrow transplant to replace damaged stem cells. Early detection and prompt treatment are essential for managing this potentially life-threatening condition (7).
Sickle Cell Anemia
Sickle cell anemia is a hereditary blood disorder characterized by abnormal hemoglobin, known as hemoglobin S (HbS), within red blood cells. This genetic mutation causes red blood cells to become rigid and sickle-shaped, leading to blockages in small blood vessels, impaired blood flow, and tissue damage. Individuals with sickle cell anemia experience recurrent episodes of pain, called vaso-occlusive crises, as well as an increased risk of infections, anemia, and organ damage. Treatment focuses on managing symptoms and complications, including pain management, prophylactic antibiotics, hydration, blood transfusions, and hydroxyurea therapy to reduce the frequency of crises. Genetic counseling and early detection through newborn screening programs are essential for optimizing care and improving outcomes for individuals with sickle cell anemia (8).
Signs and Symptoms
Anemia can have many symptoms, but there are some common ones to look out for (3). Common symptoms include fatigue, pallor, shortness of breath, weakness, jaundice, arrhythmia, chest pain, cold extremities, headaches, and paresthesias (2). Paresthesias often accompany other neurologic changes, which may indicate a B12 or folate deficiency (1). It is essential to obtain a good patient history and to pay attention to the timeline of symptoms, as well as trends in lab values. These vital clues will help determine the cause of the anemia and what treatment is necessary.
Fundamental Lab Values for Types of Anemia
When determining if a patient is anemic, we look at a complete blood count (CBC), often ordered with a cell differential count (2). For diagnosing anemia, fundamental laboratory values include (2):
Hemoglobin (Hb)
This protein in red blood cells carries oxygen throughout the body. Normal levels vary by age and sex, but generally, for adults, normal hemoglobin levels are around 12 to 15 grams per deciliter (g/dL) for women and 13.5 to 17.5 g/dL for men. Low hemoglobin levels indicate anemia.
Hematocrit (Hct)
This measures the percentage of red blood cells in the total blood volume. Average values are typically around 37% to 47% for women and 42% to 52% for men. Like hemoglobin, low hematocrit levels indicate anemia.
Mean Corpuscular Volume (MCV)
Measures red blood cells’ average volume or size. Normal MCV ranges from 80 to 100 femtoliters (fL). Low MCV (microcytic anemia) may indicate iron deficiency anemia, while high MCV (macrocytic anemia) may suggest vitamin B12 or folate deficiency.
Mean Corpuscular Hemoglobin (MCH)
This measures the average amount of hemoglobin per red blood cell. Normal MCH ranges from 27 to 33 picograms (pg). Low MCH levels may be indicative of iron deficiency anemia.
Mean Corpuscular Hemoglobin Concentration (MCHC)
This measures the average hemoglobin concentration in a given volume of red blood cells. Normal MCHC ranges from 32% to 36%. Low MCHC levels may also suggest iron deficiency anemia.
Red Blood Cell Count (RBC)
This measures the number of red blood cells per blood volume. Normal ranges are typically around 4.2 to 5.4 million cells per microliter (million/μL) for women and 4.7 to 6.1 million/μL for men. A low RBC count indicates anemia.
Red Cell Distribution Width (RDW)
This measures the variation in the size of red blood cells. Normal RDW ranges from 11.5% to 14.5%. Elevated RDW may suggest mixed causes of anemia or early iron deficiency.
Check out the chart below (2) for some fundamental lab values and their average values when examining types of anemia. Note the highlighted MCV and MCHC, which show the size and color of RBCs. These lab values are vital when reviewing a patient’s CBC and diagnosing the type of anemia the patient has.
| Indices | Description | Normal Range |
| RBC: Red blood cell count | Total # of RBCs in blood |
|
| Hemaglobin (Hgb) | Concentration of Hgb in blood |
|
| Hematocrit (Hct) | Volume of packed RBC |
|
| Mean RBC Volume (MCV) | Average size of RBC |
|
| Mean Cell Hemoglobin Concentration (MCHC) | Concentration of Hgb in the average RBC |
|

Self Quiz
Ask yourself...
- What other conditions did the last patient you cared for have along with anemia?
- Have you ever had anemia? What type? How did you treat it?
Types of Anemia Based on Lab Values
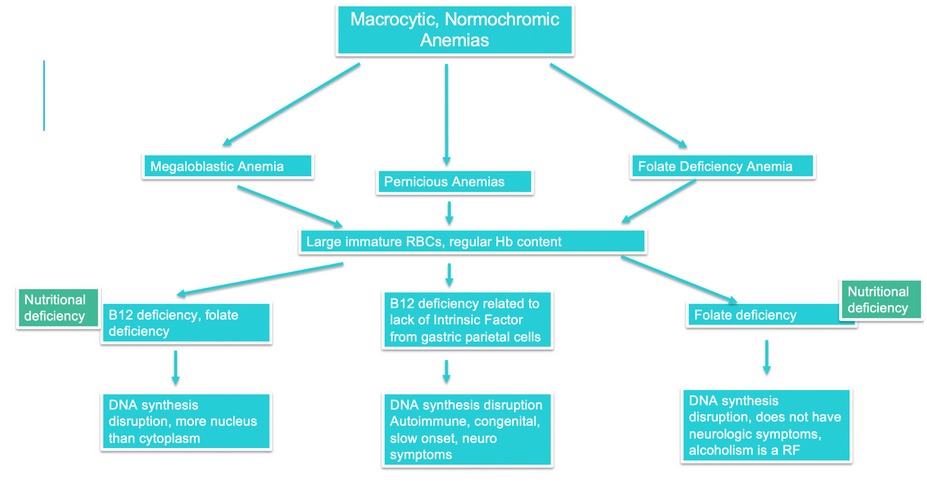
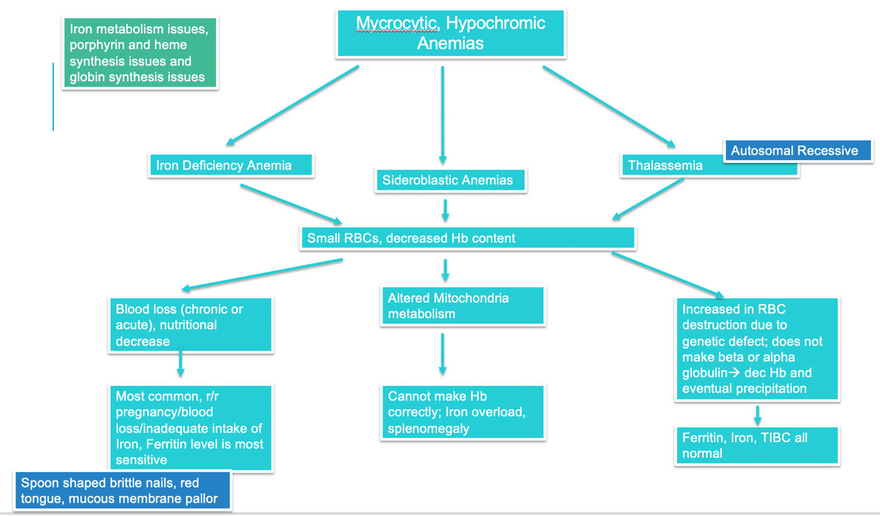
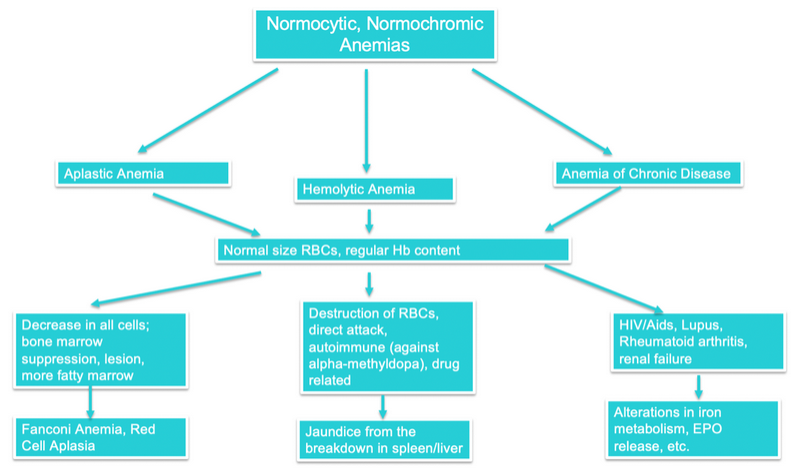
Use the following flow charts to learn the names and types of the more common anemias in response to the lab values a patient presents with. Learning how the lab values can dictate the anemia presented is useful when caring for patients.
By definition, macrocytic, normochromic anemia is one in which the RBCs are too large but have an average amount of hemoglobin. A high MCV and normal MCHC would evidence this.
In contrast, microcytic, hypochromic anemia would be evidenced by a low MCV and low MCHC. Check out the charts for what types of anemia are characterized by these lab values (2).
However, it is essential to note that there are anemias that represent a failed destruction process in which too many RBCs are destroyed, leaving the body lifeless. These are called hemolytic anemias or aplastic anemias (2, 4). In both types, RBCs are destroyed at rates too high for the body to recover.
In aplastic anemia, all cells made by the myeloid stem cell in the bone marrow are rapidly destroyed, and this is how you can identify this anemia over others.

Self Quiz
Ask yourself...
- Using the charts above, determine what type of anemia someone has if they present with a high MCV, a normal MCHC, low B12, and low folate.
- Using the charts above, determine what type of anemia someone has with a normal MCV or MCHC but is jaundiced and fatigued.
Case Study #1
A 42-year-old female presents to the emergency department with fatigue, pallor, cracked lips, a swollen tongue, and paresthesias. On discussion, you learn that she had gastric bypass surgery about two months ago. She was sent home with limited ability to get to follow-up appointments due to a lack of a car and support system. You know gastric bypass surgery can interrupt normal gastric function, and you are reminded of the parietal cells’ secretion of intrinsic factor necessary for B12 absorption. This is starting to sound like anemia related to deficiencies, but you need to confirm via labs. Her lab values are as follows:
- Hgb: 9
- MCV: 130
- MCHC: 34
Out of the various types of anemia, which do you believe she is suffering from?
Provide the type and summarize the morphology and pathophysiology.
Case Study #2
A 68-year-old gentleman presents to the emergency room with a blunted affect mirroring depression, sleep deprivation, memory loss, personality changes, and irritability. You find out during your assessment that he has a history of intermittent heavy alcohol use. You know heavy alcohol consumption can cause a decrease in normal vitamins and minerals, and you ask him about his nutritional status. It is not good. His lab values are as follows:
- Hgb: 9
- MCV: 130
- MCHC: 34
What type of anemia is he suffering from?
Provide the type and summarize the morphology and pathophysiology.
Conclusion
Anemia is a common cause for hospitalization and a common post-hospital complication. As nurses, looking beyond the hemoglobin and hematocrit values can help us work with our teams to assess and care for patients with anemia. Patients can be treated appropriately when diagnosed properly and swiftly, either in clinic or emergency department settings. The next time you care for a patient with anemia, look at their labs with a deeper understanding of what is happening at the production and/or destruction level.

Self Quiz
Ask yourself...
- What are the different types of anemia, and how do they differ regarding their underlying causes?
- Can you explain the role of iron in the body and its significance in developing iron deficiency anemia?
- How does chronic blood loss contribute to the development of anemia, and what are some familiar sources of such bleeding?
- What autoimmune disorders are associated with hemolytic anemia, and how do they lead to the destruction of red blood cells?
- What are some genetic conditions that predispose individuals to inherited forms of anemia?
- How does vitamin B12 deficiency occur, and what dietary sources are rich in this vitamin?
- Can you discuss the relationship between folate deficiency and anemia, including common risk factors for folate deficiency?
- What role does the bone marrow play in aplastic anemia, and how does damage to stem cells affect blood cell production?
- How does the body compensate for anemia, and what are the physiological mechanisms involved in response to decreased oxygen-carrying capacity?
- What are the main symptoms of anemia, and how do they vary depending on the underlying cause?
- How does the severity of anemia impact an individual’s symptoms and overall health?
- What diagnostic tests are typically performed to identify the type and cause of anemia?
- What is the significance of a complete blood count (CBC) in diagnosing and monitoring anemia?
- What is the difference between microcytic, normocytic, and macrocytic anemia, and what conditions are associated with each type?
- How do treatment approaches differ for iron deficiency anemia compared to other types of anemia?
- What are the potential side effects of iron supplementation, and how can they be managed or prevented?
- What should be considered when prescribing vitamin B12 injections for patients with B12 deficiency anemia?
- How does hemolytic anemia treatment differ depending on whether it is autoimmune-related or caused by other factors?
- What supportive measures can be implemented to manage symptoms and improve the quality of life for patients with chronic anemia?
- Can you discuss the importance of patient education in managing anemia, including dietary recommendations and lifestyle modifications?
- What are the potential complications of untreated or poorly managed anemia, and how can they be prevented?
- How do interdisciplinary collaboration and communication among healthcare professionals contribute to the comprehensive care of patients with anemia?
References + Disclaimer
- Wiciński, M., Liczner, G., Cadelski, K., Kołnierzak, T., Nowaczewska, M., & Malinowski, B. (2020). Anemia of chronic diseases: wider diagnostics—better treatment? Nutrients, 12(6), 1784.
- Lee, D. T., & Plesa, M. L. (2022). Anemia. In Family Medicine: Principles and Practice (pp. 1815-1829). Cham: Springer International Publishing
- NIH (2024). Hemolytic anemia. Retrieved from https://www.nhlbi.nih.gov/health/anemia/hemolytic-anemia on March 9, 2024.
- Kumar, S. B., Arnipalli, S. R., Mehta, P., Carrau, S., & Ziouzenkova, O. (2022). Iron deficiency anemia: efficacy and limitations of nutritional and comprehensive mitigation strategies. Nutrients, 14(14), 2976.
- Bhadra, P., & Deb, A. (2020). A review on nutritional anemia. Indian Journal of Natural Sciences, 10(59), 18466-18474.
- Bain, B. J. (2021). Blood cells: a practical guide. John Wiley & Sons.
- Alaraby, A. M., Hampshire, R. C., Frampton, C. M., Ambler, R. C., & van Rij, R. M. (2020). Anemia classification based on automated hematology analysis: The way forward. American Journal of Hematology, 95(3), E71-E73. https://doi.org/10.1002/ajh.25720
- Piel, F. B., Steinberg, M. H., & Rees, D. C. (2017). Sickle cell disease. The New England Journal of Medicine, 376(16), 1561–1573. https://doi.org/10.1056/NEJMra1510865
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate
