Course
Everything Nurses Should Know About Massive Transfusion Protocol
Course Highlights
- In this course we will learn about massive transfusion protocols.
- You’ll also learn the basics of the criteria for massive transfusions as well as common problems associated with the protocol.
- You’ll leave this course with a broader understanding of the best massive transfusion protocol practices.
About
Contact Hours Awarded: 2.5

Course By:
Janice Tazbir
RN, MS, CS, CCRN, CNE, RYT
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Massive transfusions and massive transfusion protocols are present in many institutions across the United States. Hemorrhage is the most common cause of death in the first hour of arriving to a trauma center (2). More than 80% of deaths in the operating room (OR) and nearly 50% of deaths in the first 24 hours after injury are due to exsanguination and coagulopathy (2). While only 3% of civilian, or non-military, trauma patients will receive a massive transfusion (see definition below) these patients consume an amazing 70% of all blood transfused at a trauma center (2). Knowing the basics about massive transfusions and their associated protocols can help nurses in the emergent care of trauma and other patients.
Case Study
You have recently taken a position at a Level 1 Trauma Center and are in orientation. You are excited yet intimidated by all there is to know and learn. As you come on the unit, your preceptor says, “Get ready to move, we have a multiple gunshot wound that was dropped off at the ER door and it’s our patient!”
- How do you psychologically prepare for this situation?
- How do you handle this type of stress in the workplace?
- What past experiences influence your thoughts about this situation?
- What is the first intervention that crosses your mind when hearing this case?
Introduction
Massive transfusions (MT) and massive transfusion protocols (MTPs) are a source of fear for most nurses- and for a good reason. Understanding more about massive transfusion protocols will alleviate your fear and prepare you for the time you may need it most. Every year, trauma-related hemorrhage causes four million deaths worldwide (5). Further, in the United States, trauma is the leading cause of death for all ages, particularly those under age 45. in fact, hemorrhage is the leading cause of early death following a traumatic injury (4). Uncontrolled hemorrhage is preventable yet almost one-quarter of lives have been lost (5). While applying pressure, packing wounds, and placing tourniquets may help, oftentimes bleeding may be uncontrolled and require further invasive methods (5). Over half of all in-hospital hemorrhage-associated deaths now occur after the first 24 h. Trauma in general can lead to a vast number of complications that require meticulous assessment and intervention from the medical team. In trauma, there is a deadly triad we attempt to control, consisting of (7):
- Hypothermia interferes with normal coagulation and platelet function as all chemical reactions and blood clotting are dependent on temperature.
- Acidosis is typically caused by poor perfusion related to shock (primarily hemorrhagic shock in trauma), and influences thrombus generation.
- Coagulopathy occurs with massive blood loss and is complicated if resuscitation is without coagulation factors or platelets (13).
The significance and urgency of the triad is that it will ultimately cause death if not stopped.

Self Quiz
Ask yourself...
- What other methods have you used to stop bleeding in your patients?
- How familiar are you with your facility’s massive transfusion protocol?
- What units/departments in your facility are heavily involved in massive transfusions?
- Have you ever had a patient whose presentation and lab values led you to believe they were experiencing the deadly triad?
Case Study Continued
You and your preceptor enter the trauma bay (designated area in the trauma center) and see the trauma team feverishly working. On the bed is a young man, profusely bleeding. One physician is inserting a chest tube, another is placing a femoral central line, and a third is intubating the patient. Two other nurses are helping out. Everyone is donned in full personal protective equipment (PPE). The amount of blood everywhere is daunting. The attending physician requests an MTP on the patient.
- The patient, who is Jehovah Witness, enters the trauma bay with a signed blood refusal. How does this make you feel personally, with your value system?
- What are the moral obligations you feel toward this patient?
- How do you handle a situation like this one?
- How do you maintain dignity and respect for this patient?
What Is a Massive Transfusion
A Massive Transfusion (MT) is when either (1)(6):
- 10 units or more of whole blood or packed red blood cells (PRBCs) are administered within 24 hours.
- 3 or more units of whole blood or PRBCs are administered within one hour
An Ultra-Massive Transfusion is when (6):
- More than 20 units of PRBCs are administered within a 24- to 48-hour period.
The colossal bleeding in trauma patients is one of the leading causes of death. In the past, most hemorrhage-related deaths occurred before the patient arrived at the hospital. Now, most deaths occur after the first 24 hours of hospitalization (8). Even though hemorrhage control has improved, many patients still die at some point during the clinical course (8). Up to a quarter of all patients who are admitted to the intensive care unit will die hours or days later (8). This causes the need for a reliable formula or protocol for those requiring massive transfusions. Now, there are multiple massive transfusion protocols that predict need and outline treatment for these patients.
Massive transfusion protocols can lower mortality rates and reduce the amount of blood products consumed (1)(3). MTPs are unpredictable and require preplanning and effort from the ER staff, trauma service, surgical team, blood bank, and delivery personnel (3).
Case Study
Remember, your patient is bleeding profusely. The attending physician wants to initiate a MTP and says, “We’ve got a medical student in here. Let’s review the criteria for an MTP in our center and give me a rundown on this patient.” The medical student begins, “We’ve got a John Doe about age 20 with multiple gunshot wounds, we haven’t counted. The problem ones are the shots to the right lower chest and abdomen. We are placing a right chest tube before a chest x-ray because we spotted a tracheal deviation indicative of a tension pneumothorax. The belly is actively bleeding; bedside sonography shows almost a liter in there, we already turned him, and there doesn’t appear to be a spinal injury posteriorly and no exit wounds. His heart rate is 140, blood pressure is 60/40 mm Hg. That’s an ABC Score of 4 and a shock index of 2.3.”
- How do you feel after reading this patients’ information?
- Have you ever experienced a situation in which a patient was deteriorating fast?
- What other resources, aside from scoring systems, help you judge the severity of your patient?
- Have you or anyone close to you been in a trauma situation? How might this affect your care?
Who Receives a Massive Blood Transfusion?
General Indications
About 3% to 5% of civilians and 10% of military personnel, who have undergone trauma, receive a massive transfusion (3). Other indications for massive transfusion include cardiovascular surgeries, liver transplants, and gastrointestinal and obstetrical hemorrhages (3). In general, there are no contraindications for a massive transfusion (3).
Positive ABC Score
Patients who may require a massive blood transfusion are given an assessment (via a scoring system) to determine if an MTP might need to be initiated. The assessment of Blood Consumption (ABC) is a simple, validated scoring system (1)(3). Each indicator that is present counts as a score of one (1)(3).
A score of two or more of these four indicators prompts that an MTP may be required (1)(3):
- Systolic blood pressure less than 90mm Hg
- Heart rate greater than 120 beats a minute
- Positive Focused Assessment with Sonography in Trauma (FAST) (indicating internal bleeding)
- Penetrating Torso Injury
The ABC score indicates a positive predictive value of 50% to 55%. Therefore, not all patient’s who are positive will need a massive transfusion. Additional criteria indicating the need for an MTP include (3):
- An ABC score of 2 or more points
- Persistent hemodynamic instability
- Active bleeding requiring surgery or angioembolization
- Blood transfusion in the trauma bay
High Shock Index Score
The Shock Index (SI) is the ratio of heart rate divided by the systolic blood pressure and was created to easily recognize shock in patients with seemingly “normal” vital signs (15). A patient with an SI ≥ 1.0 is at an increased risk of mortality, may need to be admitted to an intensive care unit (ICU), and may require an initiation of an MTP. The normal SI range is typically 0.5–0.7, but some research suggests up to 0.9 is acceptable (9).

Self Quiz
Ask yourself...
- What are other indications for patients to receive a massive transfusion?
- The normality of shock index scores can vary by facility. What score is considered abnormal in your facility?
- In your facility, what other indicator might trigger a massive transfusion protocol?
- Does your facility use any other scoring systems to determine the need for a massive transfusion protocol?
Case Study Continued
Remember, the patient’s ABC and shock index scores are very high. Your preceptor leans over and tells you, “With this MTP order, we identify a ‘runner’ to go get the MTP from the blood bank. The charge nurse already checked the order and called the blood bank. The labs I just sent include CBC, type and cross, PT, PTT INR, TEG (thromboelastography), platelets, ABG, BUN, Cr, and electrolytes. Let’s prime the rapid infuser and the blood will be here in less than one minute. All this information is in the protocol, and the ER, ICU, surgery, interventional radiology, blood bank, trauma, and nursing services all need to be on the same page.”
- Are you comfortable asking questions at work? Why or why not?
- How does this level of organization seem to you?
- Do you appreciate the work that is involved in creating a protocol like this one?
- How do you best retain information in protocols?
You ask, “What’s in an MTP?” Your preceptor responds, “It’s all ratios- packed red blood cells and plasma in a 1:1 ratio. Our Massive Transfusion Protocol has six units packed red blood cells, six units platelets, one unit plateletpheresis, and we transfuse through a rapid transfuser here that infuses blood up to 750cc a minute and warms the blood. We will keep on getting these MTP’s every fifteen minutes until the medical student calls it.”
“What do you mean-calls it?” you ask.
Your preceptor states, “Soon, when the patient goes to surgery, they will fix the cause of the bleeding, then the bleeding will slow down, and finally they will stop the transfusions. It’s in the protocol. The charge nurse is on the phone with the OR now communicating about the MTP, and the runner will follow the patient. We will also give a gram of tranexamic acid to help slow the bleeding.”
- How would you treat a patient in this situation if MTPs were not available?
- How do you see your role in this team?
- How can you make yourself a better team member in this situation?
- How clear is your communication in time-sensitive situations?
Indications for Massive Transfusion Protocol
Massive blood transfusion requires packed red blood cells along with select blood products. Studies show that combining packed red blood cells with other blood products (fresh frozen plasma, cryoprecipitate, and platelets) decreases the number of packed red blood cell units required (1). By using massive transfusion protocols, studies indicate that the number of patients receiving ten units of packed red blood cells or more is reduced by 40% (1). The amount of blood waste is decreased, and the costs associated with transfusion are reduced (1).
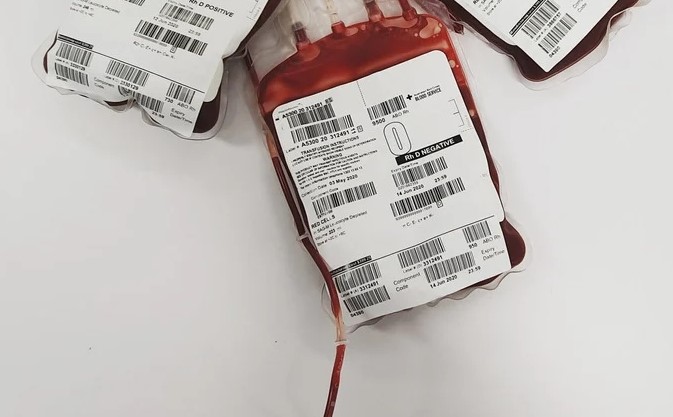
MTP packs should be available immediately once activated, include universally compatible red blood cells (O, Rh-negative, and O Rh-positive) and plasma, and be available in the ER (2).
When a patient bleeds, they not only lose blood, but they also lose coagulation factors. Only whole blood contains coagulation factors and is rarely used in institutions because of storing issues. Packed red blood cells do not contain most coagulation factors, and these factors need to be replaced concurrently during massive transfusions (2).
The 1:1 infusion ratio of plasma and packed red blood cells can help prevent exsanguination (2). The American College of Surgeons recommends a 1:1 to 1:2 plasma-to-RBC infusion ratio (2).
Each standard MTP pack will contain red blood cells, plasma, and a plateletpheresis unit, in a standardized ratio. For example, An MTP may include six units packed red blood cells, six units platelets, one-unit plateletpheresis.
The MTP is dispensed from the blood bank and physically transported by the “runner” in a designated cooler with the patient’s information on it. Blood and blood products require standard two-person verification and documentation prior to infusion.
Along with blood products, there are non-blood adjuncts used in massive transfusion and the bleeding patient (2).
Tranexamic acid (TXA) or aminocaproic acid is an antifibrinolytic medication used to inhibit plasminogen activation and plasmin activity, stabilizing clotting and decreasing bleeding (2).
Tranexamic acid is used in trauma, but also in cardiovascular and orthopedic surgery and in the case of postpartum hemorrhage. Tranexamic acid can be used as part of a protocol in trauma or given when increased fibrinolytic activity is found (2).
The recommended dose and frequency of TXA is 1 gram intravenous over 10 minutes followed by infusion of 1 gram over eight hours in actively bleeding patients within three hours of injury (2).
Recombinant activated factor VIIa was made for the treatment of hemophilia (2). Though it has been studied in the setting of trauma and warfarin-created anticoagulation, the role of factor VIIa is not clear in MTPs (2).
Prothrombin complex concentrates (PCC) contain three or four clotting factors (2). PCC is approved for warfarin-induced coagulopathy and in bleeding patients (2). Prothrombin complex concentrates are recommended to use over FFP for warfarin reversal if massive bleeding is present (2).
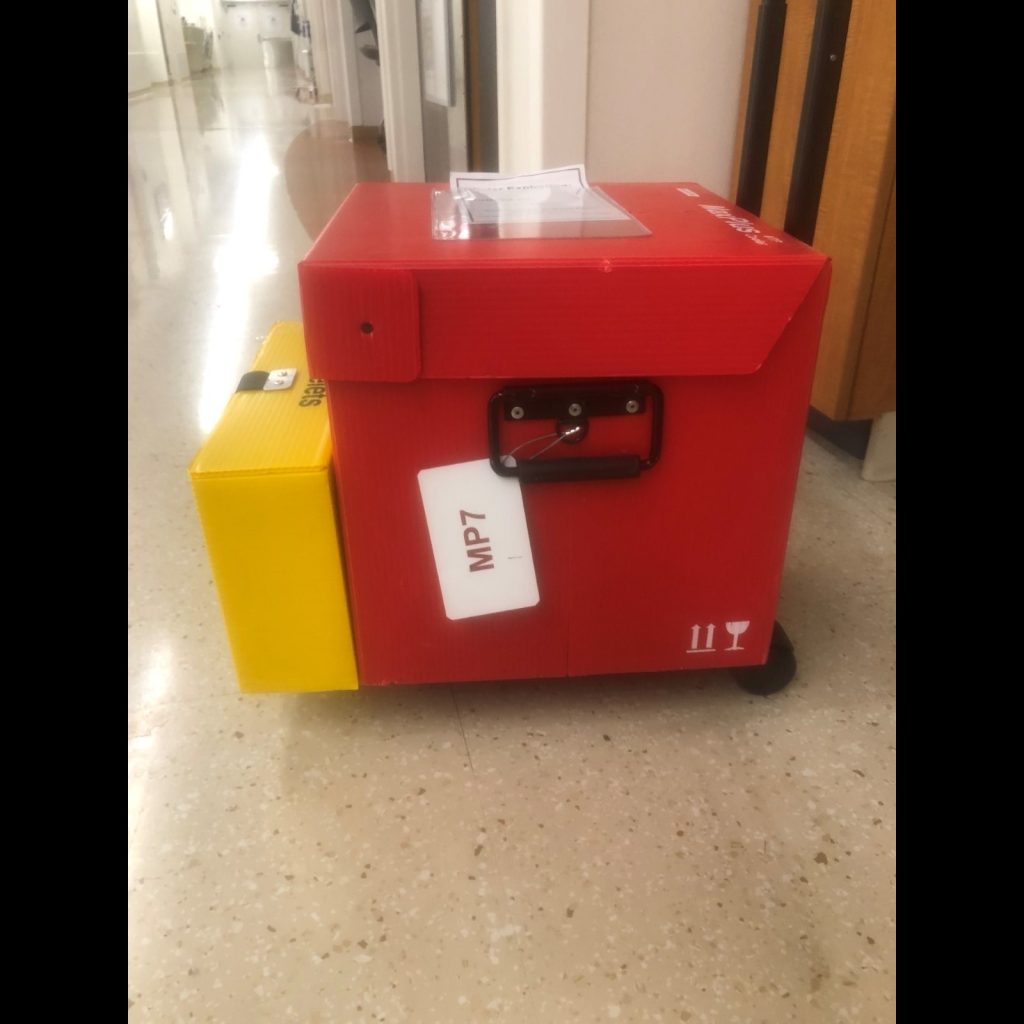
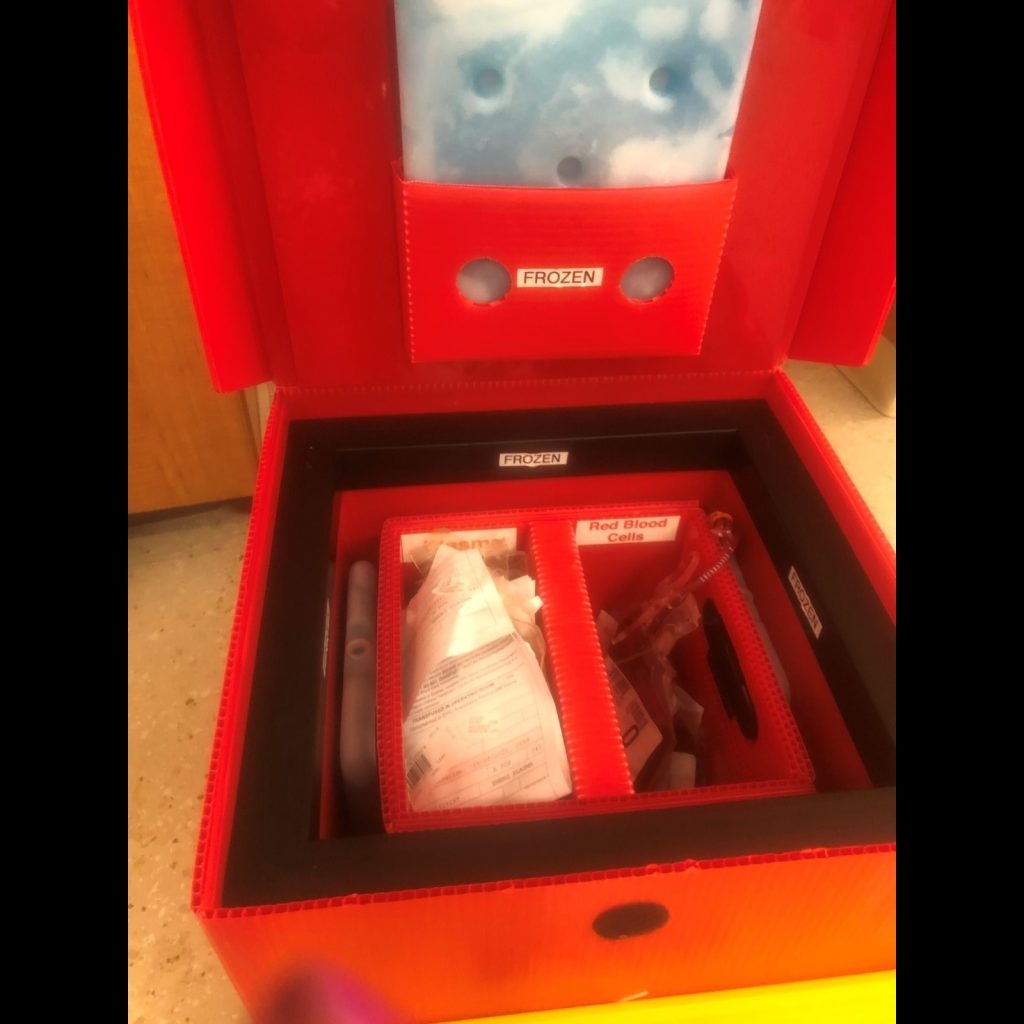
Image 1. Courtesy of J. Tazbir

Self Quiz
Ask yourself...
- How comfortable are you administering blood transfusions?
- What type of blood products do you have experience administering?
- How detailed is the process by which you obtain the blood products from the lab?
- Can you think of any other medications that may be administered during a massive blood transfusion?
Case Study Continued
After infusing the entire contents of the MTP and the arrival of a second MTP to accompany the patient to the OR, the patient is transfered to the OR accompanied by the trauma surgeons, anesthesia, and the runner.
You ask, “When they control the bleeding in surgery and send the patient to the ICU, does the patient stabilize pretty quickly?”
Your preceptor responds, “Our initial treatment and the surgery saves the patient’s life but getting an MTP can cause all sorts of problems that the ICU will have to deal with. They can have hyperkalemia, hypocalcemia, acidosis or alkalosis, hypothermia, thrombocytopenia, and transfusion reactions from all the blood that was given.”
- How do you de-stress from a traumatic situation like this?
- Are you aware of the clinical signs of hyperkalemia and hypocalcemia? List them.
- When treating patients in emergency situation, are you able to remember all the side effects of treatments?
- How will you evaluate the effectiveness of your nursing care in this situation?
Problems Associated with Massive Transfusion Protocols
There is a range of problems associated with blood product administration and massive transfusions. They generally include thrombocytopenia, acid-base imbalance, electrolyte abnormalities, hypothermia, and transfusion reactions but may be more extensive depending on the individual patient (2).
Thrombocytopenia
Packed red blood cells do not contain platelets or plasma, making patients at risk for thrombocytopenia (1). Monitor the patient and the lab values for low platelets and notify the provider if present (1).
Acid/Base Imbalance
Metabolic alkalosis may occur because packed red blood cells, platelets, and plasma contain additional acid from storage and the addition of citrate (1). When citrate breaks down, it can lead to increased bicarbonate production, and in turn, metabolic alkalosis (1). Metabolic acidosis may occur, especially if the patient is hypothermic and is part of the deadly triad in trauma.
Electrolyte Abnormalities
The citrate added to blood binds to calcium, reducing the amount of available calcium and lowering blood calcium concentrations (1). Hypothermia interferes with calcium. Ionized calcium levels are most accurate and should be monitored and reported for calcium replacement (1).
As blood ages in storing, dead cells release potassium, increasing potassium levels, and increasing the risk for hyperkalemia (1). Hyperkalemia is always a risk in patients with acute or chronic kidney injury, and elevated levels need to be reported and promptly treated (1).
Hypothermia
Blood and blood products are all stored in refrigerators or freezers. A patient’s temperature can drop precipitately infusion of cold blood products (1). Using a blood warmer helps prevent hypothermia (1). Most written protocols address hypothermia and rewarming strategies. Hypothermia may also be independently present from exposure and blood loss. Hypothermia causes coagulation problems and should be avoided at all costs in the patient receiving an MTP.
Rewarming strategies include (4):
Passive External Rewarming
- Removing blood-soaked dressings or clothes
- Increasing the room temperature wherever the patient is
- Keeping room doors shut to decrease air flow over the patient
Active External Rewarming
- Overhead radiant warmers
- Fluid/air circulating blankets
- Head covering
Core Rewarming
- Heated intravenous fluids
One of the simplest, most cost effective and clinically effective ways to warm is with the use of warmed intravenous fluids and the use of a blood warmer (4).
Transfusion Reactions
Because of the high volume of infusions and lack of initial type and crossmatch, patients are at risk for transfusion reactions (1). Transfusion reactions range from immediately life-threatening (such as hemolytic reactions) to transfusion-associated circulatory overload (TACO) (1).

Self Quiz
Ask yourself...
- How can you identify transfusion reaction in a patient who is unstable and bleeding from trauma?
- Who can help you do handle this situation?
- Which rewarming strategies have you used in the past? Which has been most effective?
- If a patient comes with trauma and is unable to give a medical history, how can you identify if the patient has renal problems?
Best Practices
The best practice for MT includes defining an MT, establishing a trigger method for initiating an MT so it can be promptly initiated through an institutional massive transfusion protocol. MTPs should use fixed ratios of blood products approximating a ratio of 1:1, including fibrinogen replacement (2). While MTPs should be made according to each facility’s clinical setting and logistic issues, all aim to achieve the same goal in providing evidence-based practices for how to manage hemorrhages with transfusions to achieve the best patient outcomes (6).
Establishing Quality Indicators
To achieve best practices, facilities should measure MTP performance by engaging in quality improvement (6). By performing audits and collecting quality indicators (QI), facilities can improve standards of care and compare practices with other organizations, nationally and globally (6).
Measuring quality indicators in transfusion care may include measuring/reporting (6):
- Rates of transfusion-related infections
- Time from MTP initiation to arrival of blood products
- Use of blood products prior to MTP
- Lab testing prior to initiation of MTP
- Number of blood products used during MTP
- MTP deactivated
- Blood product waste
- Lab investigations during MTP
- Hemostatic adjuncts
- Patient outcomes (mortality, morbidity, length of hospital stay, transfusion reactions)
Developing Protocols
MTPs should follow clinical practice guidelines, for example, the “Massive Transfusion in Trauma Guidelines” by the America College of Surgeons, released October 2014. For an MTP, quality indicators should be scientifically sound, easy to collect, and provide an actionable outcome for improvement (6). Currently, there is no evidence of which benchmarks best evaluate effectiveness (6). However, nurses can contribute to positive patient outcomes by following the protocol closely and accurately documenting all transfusions, including any adverse events and patient responses.

Self Quiz
Ask yourself...
- Who can you consult in your facility for further information about the massive transfusion protocol?
- How familiar are you with concepts of quality improvement?
- Can you think of a logistical issue within your facility that may affect the effectiveness of a massive transfusion protocol?
- If you have ever been involved in the care of patients who received a massive transfusion, what were the patient outcomes?
Clinical Guideline Recommendations
The American College of Surgeons recommends the following:
Development of a multidisciplinary committee with representatives from:
- Transfusion services
- ER
- Anesthesia
- Trauma service)
The team should develop an MTP that is easily accessible to staff.
- The activation of an MTP should include the following indicators (1):
- ABC score of two or more
- Persistent active bleeding and/or hemodynamic instability
- General recommendations for patients who require MTP include (1):
- Using a blood warmer if more than three blood products are given in a single setting
- Ongoing assessment to determine volume loss and changes in patient condition
- Evaluate need for further blood products
If MTP triggers are met (1):
- Infuse blood products instead of crystalloid or colloid solutions to avoid hemodilution and fluid overload.
- The process should include the automatic delivery of MTP coolers every 15 minutes until the MTP has been stopped.
Once major bleeding has been controlled (2):
- MTP triggers for termination are met, the MTP should be terminated, and all notified that no more MTP coolers would be required.
- Blood and blood product administration should be based on laboratory data or point of care testing
Initial baseline laboratory data should be obtained on arrival and then repeated as indicated and include (1):
- INR
- aPTT, PT
- Fibrinogen level
- Hemoglobin or hematocrit
- Platelet count
- Point-of-care testing/thromboelastometry and rotational thromboelastography (if available)
- electrolytes
- Arterial blood gases


Self Quiz
Ask yourself...
- In your facility, what is the protocol if a patient experiences a transfusion reaction?
- In your facility, who ensures that the massive transfusion protocol is being followed accurately?
- Can you think of any other labs that might be beneficial during a massive transfusion?
- How is the debriefing process in your facility after a patient receives a massive transfusion?
Case Study Continued
As your preceptor finishes going through the massive transfusion protocol in your institution, they turn to you and ask, “Any questions?”
You lean back and shake your head yes. Your fingers still slightly shaking from the whole experience, mind overwhelmed with details, you state, “This is going to take a bit to process. I’m going to start with downloading the MTP so I can really have some time to absorb it all. All I can say right now is that I sure am glad I’m on orientation, and I’m also pretty pleased this whole MTP thing was ironed out for me.”
- What are your questions after reading this?
- How will you find answers to your questions?
- How does this information inform and form your practice?
- Reflect on the interprofessional team involved in creating a massive transfusion protocol. Do you think anyone is missing?
Conclusion
Massive transfusion protocols are complex protocols that require an interprofessional team to design, create, implement and evaluate. Care of the patient who is bleeding is an intricate experience that requires a great deal of critical care knowledge. Educating yourself on this topic will allow you to further your understanding of massive transfusion protocols in your practice and better deliver care to the patients who are bleeding.
References + Disclaimer
- Adams, A. D. (2019). Massive blood transfusion protocols. American Nurse Today, 17(7), 18-20. https://www.myamericannurse.com/wp-content/uploads/2019/07/ant7-Transfusions-617.pdf
- American College of Surgeons. (2014, October). ACS TQIP Massive Transfusion in Trauma Guidelines. Retrieved from
- Jennings LK, Watson S. Massive Transfusion. [2023, October 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK499929/
- Motola, D. (2020, May 27). MASSIVE TRANSFUSION FOR COAGULOPATHY AND HEMORRHAGIC SHOCK Evidence Based Medicine Guideline [Review]. Surgical Critical Care.net. Retrieved February 24, 2021, from http://www.surgicalcriticalcare.net/Guidelines/Massive%20Transfusion%20Protocol%202020.pdf
- Jones, A. R., Miller, J., & Brown, M. (2023). Epidemiology of Trauma-Related Hemorrhage and Time to Definitive Care Across North America: Making the Case for Bleeding Control Education. Prehospital and Disaster Medicine, 38(6), 780–783. https://doi.org/10.1017/S1049023X23006428
- Sanderson,, B., Coiera, E., Asrianti, L., Field, J., Estcourt, L., & Wood, E. (2020). How well does your massive transfusion protocol perform? A scoping review of quality indicators. Blood Administration, 6, 423-424. doi:10.2450/2020.0082-20
- Van Veelen
- Brohi, K., Gruen, R.L. & Holcomb, J.B. (2019). Why are bleeding trauma patients still dying?. Intensive Care Med 45, 709–711. https://doi.org/10.1007/s00134-019-05560-x
- Koch, E., Lovett, S., Nghiem, T., Riggs, R. A., & Rech, M. A. (2019). Shock index in the emergency department: utility and limitations. Open access emergency medicine : OAEM, 11, 179–199. https://doi.org/10.2147/OAEM.S178358
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate
