Course
Endovascular Thrombectomy and Its Role in Ischemic Stroke Treatment
Course Highlights
- In this course we will learn about endovascular thrombectomies (EVT), and why nurses play an essential role in patient evaluation both pre- and post- procedure.
- You’ll also learn the basics of IV altephase (TPA).
- You’ll leave this course with a broader understanding of the key processes, risks, and success rate of EVT.
About
Contact Hours Awarded: 1.5
Course By:
Joanne Kuplicki
MA, RN, ccrn, Nc-bc
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
As healthcare professionals, we are responsible for being up to date on all the new medical advancements and treatment options available to our patients; this is no different for stroke care and, in this case, ischemic stroke treatment.
Patients who have a stroke, also known as a cerebrovascular accident, due to clotting or blockages typically will have limited medical options. For example, medication treatments with intravenous (IV) alteplase or interventional procedures like clot removal/retrieval are known as endovascular thrombectomy (EVT).
Are we as caregivers familiar with these newer ischemic stroke treatment procedures beyond the IV infusions of “clot-busters?” These interventional treatments can be done up to 24 hours post-ischemic stroke (3).
Nurses are vital in educating patients and families regarding the signs and symptoms of stroke and the options offered, as well as knowing possible contraindications, essential monitoring, and complications.
Stroke Guidelines and Incidence:
The American Stroke Association (ASA) and American Heart Association (AHA) released a 2019 update to the “2018 Guidelines for Early Management of Patients with Acute Ischemic Stroke” to reflect new clinical studies.
The guideline, which is available on the ASA’s website, enables clinicians to be aware of the recommended ischemic stroke management and treatments for improving patient outcomes after an ischemic stroke (5).
There are many acute care centers nationwide that are certified by the Joint Commission or American Stroke Association in Stroke Care that must follow these guidelines.

Self Quiz
Ask yourself...
- Are you familiar with where the nearest certified stroke center is in your area?
- Do neighbors and relatives ever ask you for referrals to the “best hospital” for ….?
Ischemic Stroke Treatment: Intravenous Tissue Plasminogen Activator (tPA) and/or Endovascular Thrombectomy
Tissue Plasminogen Activator (tPA)
An IV tissue plasminogen activator (tPA), such as alteplase, is typically ordered by the healthcare provider once a hemorrhagic stroke has been ruled out by a CT scan of the head and the patient has met the tPA inclusion criteria. This infusion must be administered by the nurse within 4.5 hours of stroke symptoms onset and is standard for most ischemic stroke patients, even if EVT is being considered as an option.
The nursing staff should have access to the complete list of contraindications and exclusion criteria. While the nurse should be aware of these contraindications and exclusion criteria, it’s still the healthcare provider’s decision and clinical judgment to order tPA. If the nurse discovers any contraindications, they should notify the healthcare provider immediately and not administer the tPA until discussed with the provider.
Some contraindications for this medication include some of the following (3):
- Acute intracranial hemorrhage or subarachnoid hemorrhage
- History of a recent stroke
- Recent head trauma
- Intracranial or spine surgery in the past three months
- Recent or active GI bleeding or malignancy
- Intracranial conditions that increase the risk of bleeding
- Severe, uncontrolled hypertension
- Oral anticoagulant use
- History of diabetes and prior ischemic stroke
- Age greater than 80 years old
- National Institutes of Health Stroke Scale (NIHSS) score greater than 25
Additional Key Points:
- The administration time frame should be as short as possible and be driven by the last time the patient did not experience or demonstrate symptoms.
- Intravenous alteplase is given at a rate of 0.9 mg/kg, and the maximum dose should not exceed 90 mg. The nurse first administers a bolus dose of 10% of the total dose over 1 minute and the remainder of the infusion is given over the next 60 minutes (3).
- Post-infusion, the patient is transferred to the intensive care unit (ICU), if not already done so, for 24-hour monitoring. The ASA guidelines recommend completing vital signs, including blood pressure control and a neurological assessment. The neuro assessment must be done every 15 minutes for the duration of the alteplase infusion and continued every 15 minutes for 2 hours after the infusion is complete. This is followed by vital signs and neurological assessment every 30 minutes for 6 hours, and every 1 hour for 24 hours (5).
- Patient’s blood pressure should be below 180/115 mm Hg for 24 hours after administration (1)
- Inserting invasive lines (like central and arterial) and urethral catheters should be delayed during immediate and post-tPA administration due to the increased risk of site bleeding (5).

Self Quiz
Ask yourself...
- Does your facility have the ability to give IV alteplase (TPA) timely?
- Are there trained practitioners, nurses and pharmacists available 24/7 to prepare and administer this IV infusion since it is time-sensitive?
Endovascular Thrombectomy (EVT)
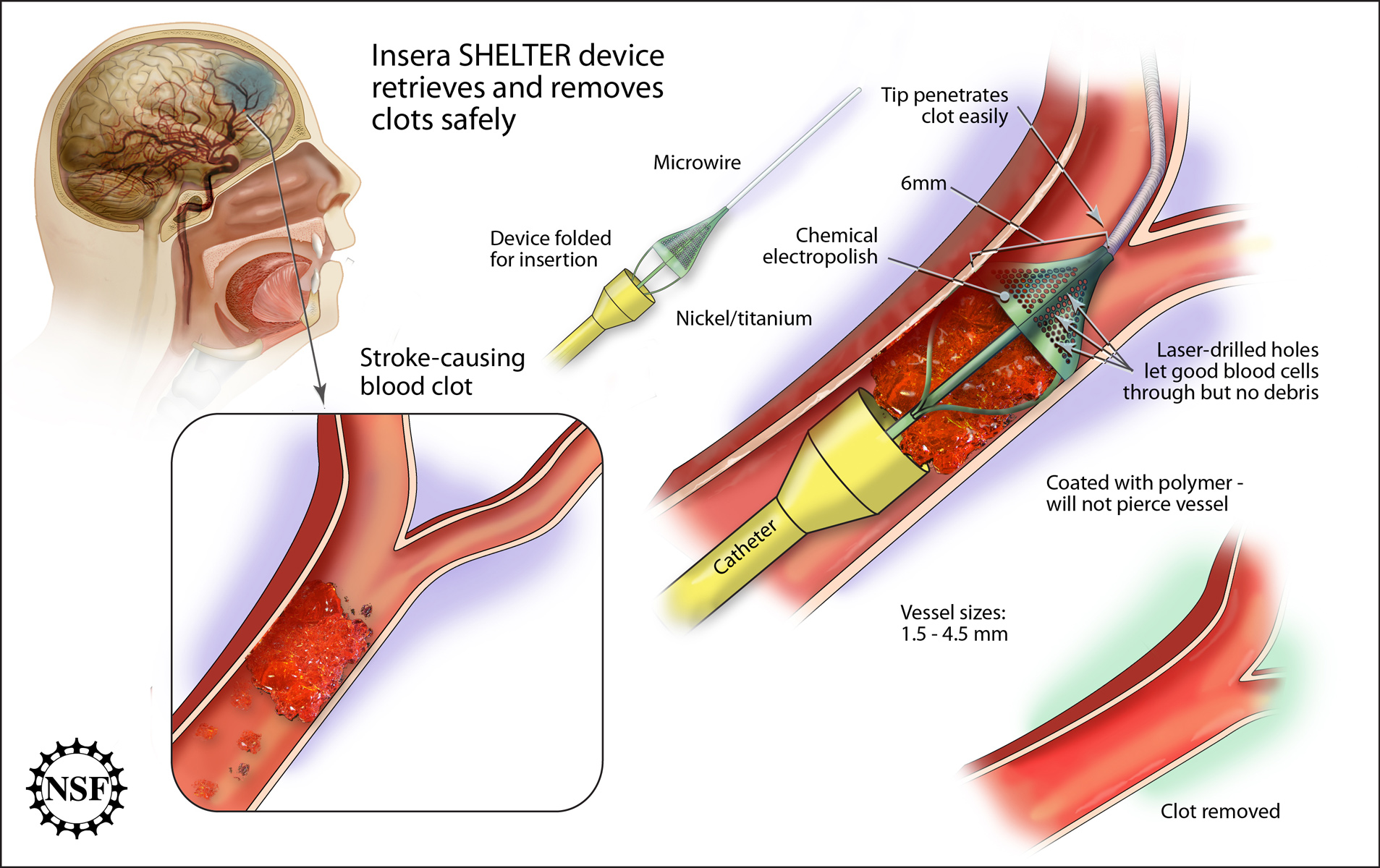
An endovascular thrombectomy (EVT) is another viable recommended ischemic stroke treatment option for patients. EVT is the removal of a thrombus or blood clot under image guidance (3). It is one of the newer ischemic stroke treatment options available to patients.
Healthcare providers should perform EVT evaluation and treatment as soon as feasibly possible for patients who meet the criteria and are eligible. However, remember that not all acute care facilities have this capability, so urgent transport options may need to be considered as well.
The time frame for EVT is recommended to be within 6 and up to 24 hours, in some patients with acute ischemic stroke (1,3).
There are specific imaging criteria that must be met:
- The occlusion must be located within a larger, more proximal cerebral vessel, usually in the anterior circulation of the brain. (Remember that most of the anterior circulation is fed from the internal carotid artery, which ends in the anterior and middle cerebral arteries. Blockage in these vessels can have devastating outcomes) (1)
IV tPA and EVT interventions are time sensitive. Healthcare organization’s processes should be in place to avoid delay from “symptoms to definitive treatment” per ASA guidelines (5).
As mentioned, the non-contrast CT scan must be done as soon as possible to rule out hemorrhage before any treatment with IV clot-dissolving medications or neuro-vascular intervention.
A finger-stick blood glucose is recommended before tPA IV administration, since glucose abnormalities can mimic stroke, as can other disorders such as drug overdoses, etc. A thorough history and physical examination are crucial, and the patient’s family and/or significant others can provide additional specific vital information (3)
Vital signs (including oxygen saturation) are done along with neurological assessments (1).
Lab work on stroke patients may include cardiac markers for ischemia (ex. troponin) and platelet count. IV tPA is contraindicated in those with platelet counts less than 100,000 mm3. PT/INR and aPTT coagulation studies are part of the initial standard of treatment. Alteplase (tPA) is contraindicated with PT greater than 15 sec, INR greater than 1.7, and/or aPTT greater than 40 (1).

Self Quiz
Ask yourself...
- Does your facility have a timely lab turnaround time?
- Has there been any improvement in this process to include unit-based phlebotomists or nursing personnel trained to draw stat and time-sensitive lab specimens?
Key Processes:
- EVT is usually completed within 6-24 hours, and up to 24 hours after the “last known well or normal” time, not from the start of symptoms. Patients who present with symptoms after sleeping can have difficulty establishing this timeframe (3).
- The patient’s Modified Rankin Score (MRS) pre-stroke should be 0-1 (out of 6), meaning a low level of existing disability before acute stroke (3).
- The CT scan with perfusion or MRI/MRA which shows brain circulation must reveal occlusion of the internal carotid artery or proximal (larger vessel width) middle cerebral artery (1).
- EVT is not an acceptable procedure for those under 18 OR for patients with an NIHSS score ≤of 6 (1).

Self Quiz
Ask yourself...
- Have you had experience either observing or performing the National institute of Health Stroke Scale (NIHSS) assessment on any potential or confirmed stroke patients?
- Do you know where to find resources quickly (for example www.stroke.nih.gov) for this vital assessment at your organization?
Potential Complications:
The entire team must be aware of potential intra-procedural and post-procedure complications. Complications should be minimized and effectively treated quickly.
Some potential complications include (4):
- Groin access site complications or infection
- Arterial vessel or nerve injury
- Hematoma
- Vasospasm
- Arterial perforation or dissection
- Device misplacement
- Rarely symptomatic intracerebral hemorrhage or subarachnoid hemorrhage occurs
- Embolic formation in the target vessel, or other areas that are listed as a potential complication
The nursing and healthcare team members are key players in monitoring subtle neurological changes, although anesthesia during the procedure can delay post-procedure accuracy. The clinical staff should have unit-based training and education on assessing groin vascular puncture sites and care, quickly controlling bleeding, assessing labs, and reporting findings promptly. Many healthcare organizations have added unit toe pulse oximetry and dopplers as additional tools to assess lower limb perfusion.

Self Quiz
Ask yourself...
- Have you ever been responsible for monitoring patients post intra-vascular procedure?
- Is there specific equipment or response team available for urgent intervention of complications (like Hemorrhage)?
- Are they available 24/7 in your organization?
Nursing Role Post- Ischemic Stroke Treatment: IV TPA and/or EVT
For patients who have undergone an ischemic stroke treatment, such as IV TPA and/or EVT, it is essential for nurses to frequently check vital signs and perform neurological evaluations, as this can work to ensure positive patient outcomes. Although this task predominately falls under the nursing role, all team members should be trained to recognize any change in signs/symptoms, including our interdisciplinary colleagues (supportive personnel, physical therapist, occupational therapist, and speech therapist, etc.).
Here are a few details all nurses should be aware of post-alteplase and/or EVT:
- If the patient’s blood pressure is greater than 180 systolic or 105 diastolic, they should be treated with an antihypertensive agent as ordered by the healthcare provider (1).
- Labetalol or nicardipine are examples of medications used for blood pressure management.
- Dysphagia evaluation early in the care of a stroke patient can determine the patient’s choking and aspiration risk. This is a critical safety step to help prevent any aspiration event.
- Aspirin is part of the ASA’s ischemic stroke antiplatelet guidelines and is to be given at a dose of 325mg orally or rectally if the patient is NPO and within 48 hours of stroke/transient ischemic attack (TIA) onset. If a patient is treated with alteplase, aspirin administration is delayed until about 24 hours later (1).
- No aspirin is given within 90 minutes after the start of IV alteplase (1)

Self Quiz
Ask yourself...
- If you work in an area that takes care of stroke patients, have you had formal training on how to perform a standardized dysphagia evaluation?
- Is this documentation part of your electronic medical record to improve the continuum of care and transfer between units?
Experience of Regional Stroke Service: Ischemic Stroke Treatment
A small research study published in 2023 reviewed the effectiveness of endovascular thrombectomy treatment from July 2018 to February 2023. The study reported improved functional outcomes for patients who underwent an endovascular thrombectomy compared to medical treatment alone. Furthermore, their mortality rates were lowered (2).
Another larger research review of 3,793 participants across 19 studies found that endovascular thrombectomy increases the chances of survival and functional outcomes without increasing the risk of hemorrhage (6).

Conclusion
Ischemic stroke treatment options have advanced beyond just medical therapies including IV tPA. The clinical team must recognize EVT as an advanced ischemic stroke treatment that is available in some stroke centers across the country. More importantly, the nurse plays a vital role in assisting the neurological team with obtaining detailed symptom presentation and time frames, as well as frequently monitoring vital and neurological statuses and being cognizant of complications and urgent interventions if needed.
References + Disclaimer
- American Heart Association. (2019). Guidelines for the Early Management of Patients with Acute Ischemic Stroke: 2019 Update to the 2018 Guidelines for the Early Management of Acute Ischemic Stroke. Retrieved from https://www.heart.org/-/media/Files/Professional/Quality-Improvement/Get-With-the-Guidelines/Get-With-The-Guidelines-Stroke/2019UpdateAHAASAAISGuidelineSlideDeckrevisedADL12919.pdf
- Bendszus, M., Fiehler, J., Subtil, F., Bonekamp, S., Aamodt, A. H., Fuentes, B., Gizewski, E. R., Hill, M. D., Krajina, A., Pierot, L., Simonsen, C. Z., Zeleňák, K., Blauenfeldt, R. A., Cheng, B., Denis, A., Deutschmann, H., Dorn, F., Flottmann, F., Gellißen, S., Gerber, J. C., … TENSION Investigators (2023). Endovascular thrombectomy for acute ischemic stroke with established large infarct: multicentre, open-label, randomized trial. Lancet (London, England), 402(10414), 1753–1763. https://doi.org/10.1016/S0140-6736(23)02032-9
- Hui, C., Tadi, P., & Patti, L. (Updated 2022, June 2). Ischemic Stroke. In StatPearls. StatPearls Publishing, Inc. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK499997/
- Pilgram-Pastor, S. M., Piechowiak, E. I., Dobrocky, T., Kaesmacher, J., Den Hollander, J., Gralla, J., & Mordasini, P. (2021). Stroke thrombectomy complication management. Journal of neurointerventional surgery, 13(10), 912–917. https://doi.org/10.1136/neurintsurg-2021-017349
- Powers, W. J., Rabinstein, A. A., Ackerson, T., Adeoye, O. M., Bambakidis, N. C., Becker, K., Biller, J., Brown, M., Demaerschalk, B. M., Hoh, B., Jauch, E. C., Kidwell, C. S., Leslie-Mazwi, T. M., Ovbiagele, B., Scott, P. A., Sheth, K. N., Southerland, A. M., Summers, D. V., & Tirschwell, D. L. (2019). Guidelines for the Early Management of Patients with Acute Ischemic Stroke: 2019 Update to the 2018 Guidelines for the Early Management of Acute Ischemic Stroke: A Guideline for Healthcare Professionals from the American Heart Association/American Stroke Association. Stroke, 50(12), e344–e418. https://doi.org/10.1161/STR.0000000000000211
- Roaldsen, M. B., Jusufovic, M., Berge, E., & Lindekleiv, H. (2021). Endovascular thrombectomy and intra-arterial interventions for acute ischaemic stroke. The Cochrane database of systematic reviews, 6(6), CD007574. https://doi.org/10.1002/14651858.CD007574.pub3
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate
