Screening and Assessment for Nurses
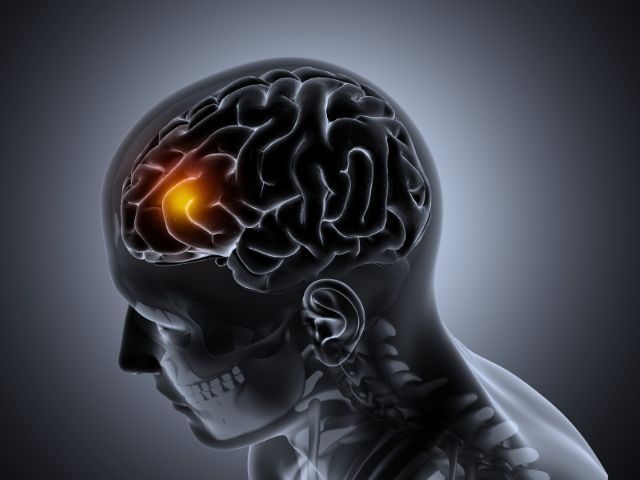
When first hearing the term ‘increased ICP’, a headache may come to mind. The real question is, ‘what differentiates a bad headache from a headache caused by increased ICP?’
For nurses, focused assessments are crucial in the prevention of disease progression. A cluster of signs and symptoms in combination with a detailed patient history may give a clue as to whether a patient’s headache is non-threatening or one that is associated with a potentially life-threatening condition, like increased ICP.
While neurological screening tools like the Glasgow Coma Scale may be useful for determining a patient’s mental alertness, critical thinking, and assessment skills are arguably the most valuable tools nurses have when caring for patients. Screening tools are intended to simply guide the nurse’s assessment.
As a medical surgical nurse, I frequently cared for patients at risk for increased ICP. In the mornings, I would perform initial head-to-toe assessments for all of my patients. However, as the shift progressed, my patients’ conditions often changed, prompting the need for continually focused assessments.
Something as simple as a patient’s report of increased pain led to my completing a focused pain assessment. Where is the pain and where did it originate? How bad is the pain? When did the pain start to get worse? What were you doing before the pain started? After obtaining subjective data, I would gather objective data – vital signs, observing for physical signs of pain, assessing the location of pain, etc.
When caring for patients with increased ICP or those at risk (recent seizure, head injury, high blood pressure, history of brain aneurysm, etc.), it is vital for the nurse to take note of any reported or observed symptoms and investigate further.
One symptom alone does not always paint the clearest picture. If there is a concern, nurses should address it with the physician and other members of the healthcare team.